Islet Transplant Program
In January 2015, the University of Louisville partnered with UofL Health - Jewish Hospital and initiated an Islet Transplant Program and successfully performed the first islet cell auto-transplant in Kentucky.
In its first year the program performed nine islet auto-transplants. The intention of the program is to help individuals suffering from chronic pancreatitis, but in the future hope to include treatment for type I diabetes. To date we have performed over 60 islet auto-transplants. The program is ongoing at UofL Health - Jewish Hospital.
The UofL Division of Endocrinology, Metabolism and Diabetes plays a key role in this program by evaluating islet function prior to islet transplantation and management of glycemic status in the immediate post-operative period and long term. We have also been involved in clinical studies evaluating islet function and long- term outcomes.
- What are islet cells?
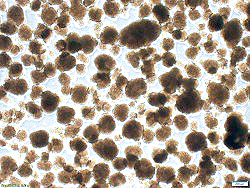 Islets are clusters of cells scattered throughout the pancreas that produce several hormones that are required for the maintenance of proper sugar levels in the body. The main function of these cells is to be able to sense blood sugar levels and respond by producing the hormones insulin and glucagon and secreting them into the bloodstream to maintain a normal blood sugar level.
Islets are clusters of cells scattered throughout the pancreas that produce several hormones that are required for the maintenance of proper sugar levels in the body. The main function of these cells is to be able to sense blood sugar levels and respond by producing the hormones insulin and glucagon and secreting them into the bloodstream to maintain a normal blood sugar level.
There are four different types of cells within an islet and each cell type has a unique responsibility for keeping proper blood sugar levels in the body. Beta cells are one class of these cells whose responsibility is the production of insulin. In individuals with Type I diabetes, these beta cells have been completely destroyed which leads to improper blood sugar levels and severe consequences to the overall health of the body.
- Why would someone need an islet cell transplant?
Chronic pancreatitis is ongoing inflammation of the pancreas that does not heal or improve. As the condition worsens over time it results in unrelenting abdominal pain and permanent damage that eventually affects the organ's ability to produce digestive enzymes and pancreatic hormones produced by islet cells. The only cure is complete removal of the diseased organ, which then leaves patients with surgically induced diabetes. This can be corrected with supplements or islet cell transplant.
- Who is affected by chronic pancreatitis?
According to The National Pancreas Foundation, chronic pancreatitis has an annual incidence rate of 5-12/100,000 people in industrialized countries. It often develops in individuals between the ages of 30 and 40 and is more common in men than women.
Chronic pancreatitis can be caused by heavy alcohol use, autoimmune conditions, blocked pancreatic duct or common bile duct, genetic mutations associated with cystic fibrosis, and familial/hereditary pancreatitis.
Symptoms of chronic pancreatitis include upper abdominal pain that sometimes spreads to the back, which can become worse after eating or drinking, nausea, vomiting, weight loss, diarrhea, oily or fatty stools, and clay-colored or pale stools. Many patients of chronic pancreatitis experience a decreased quality of life and often require admission to the hospital for treatment of its symptoms.
- What treatments are available?
 In patients where medical and pain therapy fail to provide relief from symptoms of chronic pancreatitis, surgery is the next option and typically provides pain relief in the majority of individuals. While surgical removal of the pancreas provides pain relief it also leaves patient without the ability to produce pancreatic hormones leading to surgically induced diabetes.
In patients where medical and pain therapy fail to provide relief from symptoms of chronic pancreatitis, surgery is the next option and typically provides pain relief in the majority of individuals. While surgical removal of the pancreas provides pain relief it also leaves patient without the ability to produce pancreatic hormones leading to surgically induced diabetes.
To combat this outcome, the pancreatic islets can be isolated from the removed organ, purified and reintroduced into the patient so that they may regain the ability to produce insulin a procedure termed Total Pancreatectomy with Islet Auto-Transplantation (TP-IAT).
Total Pancreatectomy with Islet Auto-Transplantation (TP-IAT) for Chronic Pancreatitis
- How does it work?
 Physicians will first diagnose the condition with a series of tests that can evaluate the structure of the pancreas. This is typically done with imaging technology such as ultrasound, MRI, or CT scans. Occasionally, blood tests are also performed which are not for diagnosis of pancreatitis but can be helpful in determining the underlying cause of the pancreatitis.
Physicians will first diagnose the condition with a series of tests that can evaluate the structure of the pancreas. This is typically done with imaging technology such as ultrasound, MRI, or CT scans. Occasionally, blood tests are also performed which are not for diagnosis of pancreatitis but can be helpful in determining the underlying cause of the pancreatitis.
Treatment is usually first approached with pain therapy using medication. Minor surgical procedures can sometimes provide relief, but when these treatments fail the next option is complete removal of the pancreas, which is then followed by islet transplantation (TP-IAT).
TP-IAT is a procedure where a team of surgeons will completely remove the pancreas from the patient and then transport the organ to another specialized laboratory where the pancreas is broken down and the islet cells contained within are isolated and purified. The islet cells are then transported back to the surgeons where the cells can be re-infused into the patient's liver so the cells can continue their intended function of hormone production.
- What are the goals and benefits of TP-IAT?
The TP-IAT procedure main benefit is an increased quality of life for the patient. By removing the diseased organ, patients will experience reduction of chronic pain and loss of dependence on pain-relieving narcotics. By reintroducing the islet cells to the individual, surgically induced diabetes is avoided and the patient’s body will continue producing pancreatic hormones needed for blood sugar maintenance.