Telehealth FAQ
ULP Telehealth Townhall
4/15/2020
Q. Can patients without the technology or capability to videoconference request a reimbursable telephone visit? I understand if a telemedicine appointment is attempted but not successful and we convert to phone (audio), that can be billed at the same level as telemedicine. I hope that is true.
A. This is correct. Document the attempt was made.
Q. There was a TeleHealth presentation recorded, where is it?
A. Recorded Grand Rounds on TeleHealth website: http://louisville.edu/medicine/tech/telehealth
Q. Are we working with the DNP students at UofL SON?
A. At this moment DNP students’ clinicals are on hold until after peak. We are developing our DNP curriculum to include more TeleHealth education.
The School of Nursing is looking to collaborate with other disciplines to further grow our TeleHealth education.
Q. Some patients have problems using BlueJeans and I am not able to see their video at times if they do not download the app. Are there any other HIPPA compliant platforms that U of L can offer?
A. Doxy.me Video Chat via the app is used by some and is reportedly easier for some patients to open. HIPAA as it relates to videoteleconferencing is temporarily not being enforced. Zoom and Skype for business can be obtained in versions that are HIPAA compliant though. Facetime is temporarily being allowed though Tiktok and Facebook Live are not approved.
Q: What exactly is the Doxy.me Doximity thing?
- They are actually TWO similar sounding but different things:
Doxy.me is actually a HIPAA compliant, free videoteleconferencing platform. Lots of small solo practitioners use it. There is a commercial version for larger groups.
https://help.doxy.me/en/articles/95852-why-is-doxy-me-free-how-do-you-make-money
While a number of ULP clinicians report having used it, it is not currently supported by IT as they are fully engaged in supporting the enterprise product (Bluejeans at present) and preparing for the EPIC roll out. Apparently on the patient end, Doxy.me is simpler than many of the alternatives. For that reason, limited use of it is being explored in select cases. Most higher functioning patients can probably be taught to manage Bluejeans (or similar products). However, once the reimbursement for audio only telephone calls goes away (as it is likely to do), we may need to consider something that is more user-friendly.
Doximity on the other hand is Doximity is a free online social media/networking service for medical professionals. Launched in 2011, the platform offers its members curated medical news, case collaboration and messaging capabilities.
Doximity is NOT a videoteleconferencing platform but has some useful features that those practicing telemedicine often find useful. For one, there is an APP available:
that allows users to send and receive faxes from their smart phones.
Also, the “Doximity dialer” can be very useful in that it lets you make telephone calls with your cell phone without divulging your cell phone number or having to dial *67. In fact, you can actually set it up such that your office phone number is displayed when making the call making it more likely that the person being called will accept the call.
https://www.doximity.com/clinicians/download/dialer
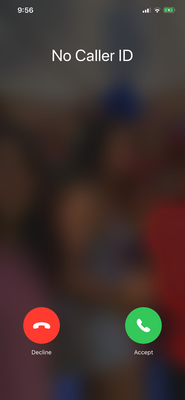
Without the app, if you use*67, the caller ID the call recipient gets a message that says “No Caller ID” that often leads them to not take the call. See screenshot below:
Q. If consulting doctors consult a specialist and you speak/exchange photos but do not come and see the patient because it is not urgent/emergent. Is it appropriate to bill a 99446?
A. It would be appropriate for you to bill 99446 if you are providing a verbal opinion and written report of your findings. For this code you do not need to see the patient, it is not the same as an evaluation and management consultation code. For this code you are verbally consulting with the referring provider and rendering an opinion from records or images that you have received via internet, phone or the EHR. This code is for 5 to 10 minutes of your time, and time does need to be documented in your report. ^
Q. I was wondering about billing telephone only visits. I have been instructed to bill based on the codes for time and the reimbursement is very low even for a 20-30 min call for a more complex patient. I had understood that insurances were going to allow for telephone visits to be billed similarly to audiovisual visits and in office visits. Is that correct and is there another way to bill a telephone only visit?
A. Insurances are providing information that they will bill the telephone visit if the attempt is made for the audiovisual visit but there are issues and you cannot make that happen. Document the attempt and it can be billed as such. Additional clarification is forthcoming on this.
Q. (2) What has been your experience doing telehealth with older adults? What has it been like providing telehealth to your older patients? Any challenges or lessons learned you can share?
A. Older patients, like their younger cohorts, have variable interest and comfort level with technology. If someone is adept at using a smartphone and knows how to download an app, they should be able to navigate the common telehealth technologies. If someone is starting to show cognitive decline, they often exhibit early impairment in instrumental activities of daily living, so it would be potentially significant if someone who was felt to be 'tech savvy' struggled with this. On the other hand, if someone never embraced smartphone technology and only used the phone function and maybe the web browser, it wouldn't be evidence of decline. In either case accommodations may be needed, such as assistance from a family member or substituting a regular phone call.
Q. I am a senior who is concerned that we may lose the relationships. So many senior adults need the touch as much as the medicine.
A. Some do. Some do not. You will definitely lose the relationship if you cannot communicate at all. During a time when COVID-19 is reportedly hitting the senior population especially hard, staying well and ultimately alive allows for relationships to recover. The current crisis will eventually pass. Many patients will prefer to return to in-person visits when circumstances so allow. For now, adapt and overcome.
Q. Any suggestions to increase patient agreeing to initial telehealth consent when you are a more elective subspecialist? Patients really enjoy our personal attention and touch and I find some are unwilling to agree to telehealth because of this
A. There really is no right or wrong answer to this as the correct answer is a varied as the patients we see. Most studies suggest that timely access ranks very high when it comes to selecting a medical service. Even initially reluctant patients when given a choice between a videoteleconferencing visit today or an in-person visit when they again become available are not surprisingly inclined to accept the earlier appointment. An entire other group of patients have historically chosen to go without services altogether due to being overwhelmed by the logistical challenges involved in finding there way to our clinics, dealing with traffic, construction, parking, and locating our offices. This group has historically been unnoticed since they rarely found their way to our offices. We now have access to them too. When the dust settles, we hopefully have a much more robust system which is far better equipped to meet patients on their own terms.
Q. What is the status of using “glasses” technology?
A. Smart glasses and other wearable videoconferencing platforms are the evolutionary descendants of “Google Glass” Steady improvements have continued to be made though Google is no longer the only manufacturer of such products. In certain settings, they may have a potential role. This is particularly true when the clinician needs to have their hands free. The smart glass gives the clinician both the heads up display of data that might be useful versus during the interaction but also a small video monitor of everything being recorded by the Go-Pro type high-definition camera built into them. For best use, they would be paired with a suitable endpoint (i.e., another professional, trainee, or supervisor who is viewing the streaming video at a separate location). Little formal study has yet been done. Certain patient populations are envisioned as being less appropriate that others to receive care from a clinician using the Smart Glass product. While “cool” to a subset of technology enthusiasts, they run the problem of giving off a zombie apocalypse vs. Borg assimilation vibe that may complicate the assessment of some patients with altered mental status. So far, the model we are testing appears to be an improvement over Google glass though a bit less stylish and clunkier though with better processing speeds and features. No getting around it though, it is high on the geek quotient. We have them though and actively pilot programs in nursing homes planned.
WEBSITE
Q: What is the URL for the UofL Telehealth website?
A: http://louisville.edu/medicine/tech/telehealth
But since you’re reading this answer on-line, you already figured that out.
TECHNOLOGY
Q: Should we avoid Zoom? I’ve heard it is now notoriously insecure and has been banned by Google/NYC Schools/multiple others.
A: No. This is an organic process and is often a repeated pattern in technology. Hackers are part of the technology ecosystem. When a company grows to a certain size, it inevitably attracts the attention of hackers. Hackers have limited time as do we all. They will generally not bother hacking platforms that are inconsequential. The rapid growth of Zoom in the face of the virus response put them on hacker’s radars. Hackers then did them the great service of exploiting their various security weaknesses thus identifying them to the programmers. Zoom’s rapid growth provided them with the financial resources to go about patching the vulnerabilities. In the end, Zoom winds up with a better product all around with the hackers having provided the company with the benefit of identifying vulnerabilities. They provide this service free of charge or in Zoom’s case with the minor expense of a short-term PR hit. Whoever had initially wound up on top will become a target. It just happened to be Zoom.
Q: Does Zoom have the advantage over BlueJeans regarding admitting people into the room?
A: Zoom and BlueJeans are competitors in the market. The feature of being able to selectively admit individuals from a virtual “waiting room” into a virtual “meeting room” does have clinical and administrative usefulness. There are advantages to having a single APP across all clinics in terms of standardization and volume pricing. We cannot comment specifically on the pricing structure but early on BlueJeans seemed to have the edge. That does not mean we will get Zoom or that BlueJeans will not add these features. At present, we are using BlueJeans. Nevertheless, it is a fluid situation and subject to change. The feature of the clinician having control over who is allowed into a given meeting space is certainly advantageous for clinical use.
Q: I’ve noted some patients seem more reluctant to use a smart phone and prefer their land line telephone. How should we address that?
A: We should be as patient as possible. Patients and clinicians are both undergoing unprecedented change in their approach to the use of communications technology. Historically, clinicians were not reimbursed for services provided via telephone (audio only) communications. This was a historical mistake and one we have long lived with. In either case, with the advent of audio-video communications, we have made the case that we should be reimbursed for these sorts of interactions. We are currently in a gray zone where due to the pandemic, audio only communications are also being reimbursed. We should perhaps consider this to be a bridge to the next level. We can meet those reluctant patients where they are for now with the expectation that we will one day soon either transfer them back to in person care or perhaps video enabled visits. This will give them a chance to start to acclimate to this environment. At the end of the day though, we should be encouraging and supporting patients in their movement toward acquisition of devices that will allow them to communicate with us with both audio and video. It is a better experience than audio only and it is uncertain how long the current reimbursement arrangements will remain in place.
Q: So what software/program/APP should we be using? I keep hearing about BlueJeans, and now Zoom. Then there’s this Microsoft Teams thing. I’m confused.
A: BlueJeans is our standard for now. Other options are being considered. The eventual switch to EPIC as an EMR may have implications as to which video teleconferencing platforms will best integrate with a new EMR. The jury is still out at the moment. Watch this space for any new developments.
Q: Do you do anything special regarding identity confirmation on new patients to assure their identity?
A: While a patient attempting to impersonate another patient is a possible (if unlikely) event, this could also occur in-person. Clinicians should still verify the identity of anyone who is unfamiliar to them from previous encounters. Standard forms of photo ID can be requested and held close enough to the camera to serve this purpose. Some caution
though should be exercised. Not everyone is so unfortunate as to actually look like their photo on a driver’s license (that’s a joke BTW). Having said that, one need not have a higher standard for patient identification over video than one would employ for an in-person visit. The standard of care is exactly the same.
RESIDENT / STUDENT TEACHING
Q: What about resident integration and supervision-considerations?
A: There may some variation from specialty to specialty with the “primary care exemption” being the most notable feature. All who are responsible for supervising the clinical work or residents would already be well familiar with the document below:
In the current environment, there is great latitude with regard to how you arrange this. Obviously both resident and attending should speak with the patient. Ideally both resident and attending will actually see the patient over video if that modality exists. This could go many ways after the crisis is resolved. Those of you interested in advocacy may want to help us see to it that the ability to train residents in providing care over virtual means is preserved after the pandemic has resolved. Telemedicine will certainly be part of their future.
Q: The medical school’s standardized patient lab is developing a “telemedicine standardized patient case. Does anyone have input or feedback for how that can be successful?
A: This is exciting to hear. This is clearly something patients and students are going to want in the future. Our ability to train students and residents in providing care using communications technology bodes well for our school. The telehealth program will be working closely with those developing this experience. See Russ Farmer and John Dickens for ideas about how to make this as meaningful as possible.
Q: Can we do distant supervision in primary care?
A: Currently, through June 30, 2020 we can do distant supervision in primary care. Dr. Kubiak thinks this extends to others without the primary care exception, although she is not as sure about that. What that means is that residents can stay home and attendings can be elsewhere. Using BlueJeans, attendings are able to enter the encounter with the patient and precept.
Q: How does this work in terms of evaluating resident competencies?
A: It appears that the AC GME has made allowances for this in most programs and will all our attendings to work with residents and students in terms of evaluating competencies.
Q: Would this have a revenue implications when working with trainees?
A: Yes! There may be positive revenue implications when attendings are able to beam in and join with trainees in the evaluation of cases. Ophthalmology, ENT, neurosurgery, surgical post-op supervision all come to mind as potentially areas to reduce lost revenue. Proper documentation is always will be key.
Q: Are there any changes in the teaching physician rules?
A: Yes. From CMS-1744-IFC via AAMC. The requirement of physical presence of the teaching physician during the key or critical part of the service can be met through direct supervision through virtual means, i.e., real time audio and video communication that allows the teaching physician to interact with the resident • Teaching physicians will be able to bill for the following services of residents provided that the resident is under the direct supervision of the teaching physician through virtual means:
· All levels of evaluation and management services under the primary care exception (PCE) provided in primary care centers
· Interpretation of diagnostic radiology and other diagnostic tests. The teaching physician must review the resident’s interpretation.
· Psychiatry services
These exceptions do not apply in the case of surgical, high risk, interventional, or other complex procedures, services performed through an endoscope, and anesthesia services. CMS asks for comments on this. •
Q: What happens if a resident is under quarantine but is otherwise able to furnish services that do not require face-to-face patient care, such as reading results of tests and imaging studies?
A: Medicare will allow billing for teaching physician services if the resident is under direct supervision via virtual means.
Q: What about moonlighting?
A: Moonlighting residents will be able to bill provided that the resident is fully licensed to practice, and the services are not performed as part of the approved GME program. This provision is mostly applicable to fellows.
REVENUE RESOURCE
Q: Is there a source that outlines current major payers and their stance on reimbursement for telehealth?
A: Good question. Reminder, we are in a very fluid environment. The following links seem to be useful in terms of following changes brought about by the virus response:
Work with your billing personnel make sure you are up to date. Many of these changes cannot be easily reversed. The ones that can and will be reverse will still have to be phased out. This will not be a simple process. Watch this space for updates.
Q: Will there be a research into patient satisfaction OR increases in RVU/efficiency/referrals with telehealth use response?
A: Yes. This area is right for scholarly work. Other universities across the country of course will be looking for opportunities here as well that we have some advantages here at U of L. R telehealth offices been up and running for many years. We are forming a Scholars group of residents and medical students who will hopefully be led by attendings interested in shepherding them toward publication. We are running a nationwide experiment whether we intended to or not. The question is can we capture the data and report out in a meaningful way. Watch this spot for further developments. Please let us know if you are interested in active participation in this endeavor.
CLINICAL APPLICATIONS
Q: What departments are most frequent users in UL Health presently. Can we have contact people within these departments to seek pointers?
A: Psychiatry and neurology have been the early leaders in this area. Psychiatry is the low hanging fruit of telemedicine in that minimal instrumentation is required and much of that work is done through means that are easily replicated in the virtual environment. Neurology has paved the way in their tele-stroke programs. Both are eager to share their expertise with others and help keep the University of Louisville on the map in this the virtual environment. Feel free to reach out directly to Dr. Robert Caudill at Robert.Caudill@louisville.edu. He has made this the focus of his academic work and looks forward to helping those in other specialties tailor the technology to fit their needs.
Q: Can these tools be used with chronic medical conditions like diabetes?
A: Yes, members of this group report that it has worked well for their diabetic patients - especially those who can download data from their pumps and glucose sensors. The Department of Urology has also been using telehealth successfully
Q: Are there other areas where we can extend telemedicine programs?
A: Yes! Cardiology among others see many opportunities to grow their practices via telemedicine. It is quite easy to add patient appointments at short notice. Treatment of gestational diabetes is also an area where telemedicine has much to offer.
Q: What about an attestation statement? What do we need to modify if anything?
A: Psychiatry has been successfully using the following attestation for a number of years. Feel free to adapt to your own specific needs if you find that necessary:
“I was face-to-face with the patient via videoteleconferencing technology. I reviewed the documentation by the resident. I provided a unique, billable service to the patient. See resident's note for details. I saw and evaluated the patient and agree with the resident's findings and plans as written.”
For attestations for audio only telephone calls, we have been using”
“I spoke with the patient via telephone. I reviewed the documentation by the resident. I provided a unique, billable service to the patient. See resident's note for details. I saw and evaluated the patient and agree with the resident's findings and plans as written.”
This of course assumes that you do in fact agree with the resident’s findings and plans. If you have differences, you will need to resolve them in the attestation or else have the resident correct their report to include statements you do in fact agree with. That is no different however then what you would be doing in person.
Q: What is the best practice for sending out meeting rooms for patients in BlueJeans?
A: Here is another moving target. Different solutions have been proposed. If you think about your current physical space, there is no guarantee that a patient cannot ever intrude upon your physical space unintentionally. For example, those of us having exam rooms on a shared hallway know that a patient could accidentally walk in the wrong room at any time. This is no different in the virtual world. Some programs are better than others about protecting the space. Zoom in particular makes use of a virtual waiting room. Patients trying to join a virtual meeting room, accumulate in a virtual waiting room and have to be admitted individually into the meeting space. On the other hand, BlueJeans does not have this feature as yet. Nevertheless, if a patient were to inadvertently intrude upon a clinical encounter, you would do exactly as you would in the real world and ask them to exit and wait until it is their turn. The idea of creating a unique blue jeans ID meeting for each and every individual patient encounter seems to be unimaginably labor-intensive. Better solutions exist.
FOLLOW-UP
Q: Do you plan to do any more of these?
A: We will continue to meet so long as sufficient number of attendees find them useful. Champions should plan to attend a 2nd meeting on Wednesday evening, April 22 at 5:30 PM. Members of the champions group will receive an invitation to their official email address.
An organization wide Zoom Telehealth Townhall is scheduled for Wednesday evening, April 15 at 5:30 PM. All ULP clinicians are invited - both AMG and CMG. A small panel will take questions regarding telehealth from the audience. Information on joining this Webinar style meeting will be publicized soon.
Q: is that all?
A: No. Our intention is for this to be a dynamic website that is updated regularly. Some answers will seem less relevant over time and new questions will arise. Please email with any questions you would like to see answered. If the question is of general interest, we will post it here.
Tim Bickel for general Telehealth questions
Dr. Caudill for clinically specific requests