News
Forging a new PATH to optimal aging
Exploring a new intervention to help older adults age optimally is the focus of the Sept. 14 lecture to kick off the second year of the Optimal Aging Lecture Series, sponsored by the University of Louisville Institute for Sustainable Health & Optimal Aging and the UofL Alumni Association This lecture is part of the Insitute’s Optimal Aging Month observance.
Valerie Lander McCarthy, Ph.D., R.N., associate professor at the UofL School of Nursing, will present a conversation entitled “Which PATH Will You Choose?” The event will be held from 11:30 a.m. to 1 p.m. at the University Club, 200 E. Brandeis Ave.
McCarthy will share a new intervention called the Psychoeducational Approach to Transcendence and Health (PATH) Program. Developed by McCarthy and her colleagues, the program fosters self-transcendence to help older adults improve well-being, life satisfaction and health-related quality of life. The program utilizes mindfulness experiences, group processes, creative activities and brief independent at-home practice.
McCarthy teaches community health nursing and evidence-based research in the undergraduate program of the School of Nursing. Her research is focused on successful aging and increasing well-being, life satisfaction and health-related quality of life in older adults through promoting the late-life developmental process of transcendence.
Admission is $30 per person and includes lunch. Reservations are required online. Click here to register. For information, call 502-852-5629 or email OptimalAging@louisville.edu.
Toni Ganzel to participate in national deans' panel on medical education, live-streamed Sept. 8 at noon
Dean Toni Ganzel, M.D., M.B.A., will discuss the future of American medical education in the National Deans’ Panel On Thursday, Sept. 8 from noon to 1:30 p.m., hosted by the University of Florida College of Medicine. The event is part of its 60th anniversary celebration. Ganzel will be joined by fellow medical school deans Joseph Kerschner, M.D. of the Medical College of Wisconsin, E. Albert Reece, M.D., Ph.D., M.B.A. of the University of Maryland and Michael Good, M.D., of the University of Florida to discuss contemporary issues in medical education, biomedical science and American health care.
Join the live stream of the event online at: http://bit.ly/DeansPanelUF
Submit questions to the panel during the event via Twitter using the hashtag #UFMed60.
How smart is the spinal cord? Andrea Behrman will explain at Beer with a Scientist Sept. 14
Andrea Behrman, Ph.D., professor in the Department of Neurological Surgery at the University of Louisville, will discuss research and progress in helping children recover from spinal cord injuries at the next Beer with a Scientist. Her research using locomotor training represents a paradigm shift in helping children with spinal cord injury regain mobility below the level of the lesion. She designs therapies based on scientific evidence that the central nervous system changes through training, a process known as activity-dependent plasticity.
Behrman is director of the Kosair Charities Center for Pediatric NeuroRecovery and co-director of the Reeve Foundation NeuroRecovery Network.
The program begins at 8 p.m. on Wednesday, Sept. 14, at Against the Grain Brewery, 401 E. Main St. A 30-minute presentation will be followed by an informal Q&A session.
The Beer with a Scientist program began in 2014 and is the brainchild of UofL cancer researcher Levi Beverly, Ph.D. Once a month, the public is invited to enjoy exactly what the title promises: beer and science. Follow the link to see a video about a recent Beer with a Scientist event with UofL professor John Pierce Wise, Ph.D.
Admission is free. Purchase of beer, other beverages or menu items is not required but is encouraged.
Organizers add that they also encourage Beer with a Scientist patrons to drink responsibly.
For more information and to suggest future Beer with a Scientist topics, follow Louisville Underground Science on Facebook.
NEXT BEER WITH A SCIENTIST, OCT. 12:
As part of Research!Louisville, Beer with a Scientist founder, Levi Beverly, Ph.D., will present: "The cutting-edge ways that researchers and clinicians are diagnosing and curing cancer right here in Louisville." Beverly will give a series of short presentations on some of the research and clinical trials happening right here in our own backyard.
September 6, 2016
School of Medicine faculty named editors-in-chief of two peer-reviewed journals
The University of Louisville continues to demonstrate international leadership in medicine as two faculty members have been named editors-in-chief of two peer-reviewed journals.
William Tse, M.D., director of Bone Marrow Transplantation at the University of Louisville James Graham Brown Cancer Center, has been named editor-in-chief of the International Journal of Transplantation Research and Medicine (IJTRM).Heidi M. Koenig, M.D., professor in the Department of Anesthesiology and Perioperative Medicine, has been named editor-in-chief of the Journal of Medical Regulation (JMR).
IJTRM is a peer-reviewed, open-access journal covering research in tissue and organ transplantation and hematopoietic stem cell transplantation. It also publishes research articles in the field of transplant rejection, immunosuppressant drugs, matching techniques, human genetic variability, transplant infectious diseases, therapeutics for human diseases, device-oriented aspects of transplantation, genetically engineered cells for transplantation, transplant complications and applications, transplant ethics and policy and more.
JMR is published by the Federation of State Medical Boards (FSMB), an organization representing the 70 state medical licensure boards in the United States and territories. State medical boards license and discipline allopathic and osteopathic (M.D. and D.O.) physicians and, in Kentucky and other jurisdictions, other health care professionals. The quarterly, peer-reviewed journal features research and articles of interest to members of medical boards and individuals interested in medical licensing and regulation.
About William Tse, M.D.:
 Tse was named director of the bone marrow transplantation program and the Marion F. Beard Endowed Chair in Hematology Research in the UofL Department of Medicine in September 2014. Tse was on the faculty at the University of Colorado Denver, where he was the director of translational research program for bone marrow transplantation and hematologic malignancies. He also previously was with Case Western Reserve University and the Fred Hutchinson Cancer Research Center/University of Washington Medical Center.
Tse was named director of the bone marrow transplantation program and the Marion F. Beard Endowed Chair in Hematology Research in the UofL Department of Medicine in September 2014. Tse was on the faculty at the University of Colorado Denver, where he was the director of translational research program for bone marrow transplantation and hematologic malignancies. He also previously was with Case Western Reserve University and the Fred Hutchinson Cancer Research Center/University of Washington Medical Center.
He was honored “the Top Cancer Doctors from United States of America in 2015” by Newsweek Magazine, Top Medical Oncologist in 2014; Leadership Development Program Award from American Society of Clinical Oncology in 2012; T. Franklin Williams Scholar Award from American Association of Specialty Professors in 2006, among other awards.
Tse is active in national organizations, serving in several capacities with the American Society of Hematology, including section chair for the annual meeting’s Oncogene Section and bone marrow transplantation outcome section, as well as the American Society of Clinical Oncology as an annual meeting abstract reviewer and the section chair on geriatric oncology.
Tse also serves leadership roles on several other journal editorial boards including as the senior editor of the American Journal of Blood Research, stem cell biomarkers section editor for Biomarker Research, senior editor of the American Journal of Stem Cells and academic editor of PLoS One.
A graduate of the Sun Yat-Sen University School of Medicine in Guangzhou, Guangdong, China, he did a thoracic surgical oncology residency at Sun Yat-Sen University Cancer Center before completing postdoctoral research fellowships in medical biophysics, immunology and cancer at the Princess Margaret Hospital/Ontario Cancer Institute and the Hospital for Sick Children in Ontario, Canada. He completed clinical pathology and internal medicine residencies at North Shore-Long Island Jewish Hospital before undertaking a senior medical fellowship in clinical research and medical oncology divisions at the Fred Hutchinson Cancer Research Center at the University of Washington Medical Center.
About Heidi M. Koenig, M.D.:
 In 2015, Koenig joined the FSMB Editorial Committee, which provides editorial guidance for JMR. Upon the retirement of the previous editor earlier this year, Koenig was named editor-in-chief of JMR.
In 2015, Koenig joined the FSMB Editorial Committee, which provides editorial guidance for JMR. Upon the retirement of the previous editor earlier this year, Koenig was named editor-in-chief of JMR.
“I hope to use my extensive knowledge of the various functions of the FSMB to the fullest by serving on the editorial committee,” Koenig said. “We are a small but growing journal and are working toward a greater online presence as well as becoming indexed.”
A journal is indexed if its articles are listed in a database such as PubMed or MedLine.
Koenig, who joined the UofL faculty in 2004, was named to the Kentucky Board of Medical Licensure in 2013 and has served on that board’s task forces on Standardized Minimum Sanctions and Telemedicine and as the board’s representative to the Kentucky Board of Nursing APRN Council. In addition to licensing and regulating physicians, the Kentucky Board of Medical Licensure regulates the practice of physician assistants, surgical assistants, athletic trainers and acupuncturists.
Koenig has been an active member of the Kentucky Society of Anesthesiology, serving as president from 2010-2014. She is author of more than 30 peer-reviewed publications in basic and clinical sciences. She gained editorial experience as an ad hoc editor for Metabolism, Anesthesia and Analgesia, Journal of Neurosurgical Anesthesiology, British Journal of Anaesthesia and Journal of Clinical Anesthesiology.
Answering the call for LGBTQ health equity
At least once a day, the University of Louisville LGBT Center receives a call from a person asking for the name of an LGBTQ-friendly physician. Lesbian, gay, bisexual, transgender and queer (LGBTQ) individuals often report that they avoid the health care system because they experienced discrimination in a medical setting. This can lead to poorer health outcomes for these individuals.
“The community needs more health care providers who fully understand what it means to be affirming to members of the LGBTQ community, and we need a way to let the community know how to find them,” said Stacie Steinbock, director of the Health Sciences Center satellite office of the UofL LGBT Center.
Physicians and other health care providers will learn specific skills for the care of LGBTQ patients at the LGBTQ Health Summit, Monday, Sept. 12 at the UofL School of Medicine. They also will have the opportunity to join a web-based network of LGBTQ-friendly providers to give potential patients a resource for finding affirming care.
Jennifer Potter, M.D., advisory dean and director of the Castle Society at Harvard Medical School and an international expert on LGBTQ and women’s health, will facilitate workshops on how to take a sexual history appropriate for persons of all sexual orientations and gender identities, and how to identify personal biases and develop skills for responding productively to witnessed micro-aggressions in the health care environment.
In addition, physicians and other practitioners will participate in a community forum and small group discussions with LGBTQ community members to enhance providers’ understanding of this patient base. The day-long symposium also will address hormone protocols for transgender patients and converting medical educational materials to scholarship.
“Historically, LGBTQ health has not been part of any health care or medical school curriculum,” said Suzanne Kingery, M.D., assistant professor of pediatrics at UofL. “It is only recently that a handful of medical schools, with UofL at the forefront, have started to do this kind of training. This health summit is a wonderful opportunity for health care providers to learn about LGBTQ care so they can provide affirming care for their patients and follow best practices.”
The event is part of the eQuality project at UofL, which works to improve health care and health equity for LGBTQ individuals, those who are gender non-conforming (GNC) and persons who experience differences in sexual development (DSD). The project began in 2014 with the mission to develop and implement a comprehensive curriculum for the UofL School of Medicine that requires students to learn, practice and demonstrate knowledge and attitudes required for excellent care of these patients.
The LGBTQ Health Summit begins at 8:30 a.m. Sept. 12 at the UofL School of Medicine. The event is sponsored by the UofL School of Medicine Office of Undergraduate Medical Education, Office for Community Engagement and Diversity, and LGBT Center. All workshops offer continuing education credit for physicians and nurses. Register for the workshops individually at https://goo.gl/CqMdEl.
Congressman John Yarmuth to offer insight into federal funding for science at UofL
When the federal government reduces funding for scientific research, labs may close and researchers may lose their positions. However, researchers have a voice in the funding process, and legislators want to hear from them.
“Scientists should be involved, stay informed and advocate for science funding,” said Naomi Charalambakis, a graduate student in the University of Louisville Department of Anatomy and Neurobiology. “A lot of students and postdocs are completely unaware of how the budget begins and where scientists can intervene to help that process along. We have direct input and we can change the attitudes of policymakers.”
To help students and faculty at UofL gain a better understanding of the budget process and how individual researchers can affect it, the Science and Policy Outreach Group (SPOG) will present, “Funding Your Future: A forum discussing the federal budget and the importance of science advocacy,” at 10:00 a.m. August 26 at HSC Auditorium.
The event’s keynote speaker, Congressman John Yarmuth, will help clarify the federal budget process and provide an update on federal funding for the 2017 fiscal year, which begins October 1. Yarmuth, who represents Kentucky’s 3rd Congressional District in the U.S. House of Representatives, serves on the Committee on Budget and the Committee on Energy.
Forum schedule:
• 10 a.m. - Naomi Charalambakis, graduate student and Society for Neuroscience fellow, “The Federal Budget – How it works and why students should care.”
• 10:45 a.m. - William Guido, Ph.D., chair of the Department of Anatomical Sciences and Neurobiology, “The Importance of Advocacy – a chairman’s perspective.”
• 11:00 a.m. – Jon Klein, M.D., Ph.D., vice dean for research of the UofL School of Medicine, will introduce Congressman John Yarmuth. A Q&A session will follow.
The event is hosted by the Science and Policy Outreach Group (SPOG) and the Career Research Advancement Focused Training (CRAFT) Seminar Series. SPOG is an organization of graduate students at UofL with the mission to create and facilitate a dialogue between students in the sciences and members of Congress and the community. The CRAFT Seminar Series offers monthly presentations on career development for postdoctoral fellows and graduate students at UofL.
UofL a site for patients who might be candidates for new drug therapy for peripheral T-cell lymphoma
iCell Gene Therapeutics announced Aug. 11 that the Food and Drug Administration has granted Orphan Drug Designation for its chimeric antigen receptor engineered T-cells directed against the target protein CD4 (CD4CAR) for the treatment of peripheral T-cell lymphoma (PTCL).
William Tse, M.D., chief of the Blood and Marrow Transplantation Division, Department of Medicine at the University of Louisville School of Medicine, said “We are very excited to have this opportunity to partner with iCell Gene Therapeutics to lead the efforts of preparing this cutting-edge immunotherapy into first-in-human clinical trial for patients suffering this extremely difficult-to-treat T-cell lymphoma.”
The Orphan Drug Designation program provides orphan status and associated development incentives, to drugs and biologics intended for the safe and effective treatment, diagnosis or prevention of rare diseases or disorders that affect fewer than 200,000 people in the United States.
Yupo Ma, M.D., Ph.D., professor of pathology at Stony Brook University and chairman and chief scientific officer at iCell Gene Therapeutics, said, “CD4CAR could significantly enhance currently available treatment options for these patients. The Orphan Drug Designation is an important achievement as we advance our development plans for this promising treatment in T-cell hematologic cancers.”
For information about CD4DAR treatment for T-cell lymphoma at UofL, contact CTOinfo@louisville.edu.
About CAR T-cell Technology
A "chimeric antigen receptor" (CAR) engineered T-cell is a patient's T-cell (a component of the immune system) that has been genetically modified to express a protein on its surface with the capability to bind to a target protein on another cell. Upon binding the target protein, the CAR protein will send a signal across the cell membrane to the interior of the T-cell to set in motion mechanisms to selectively kill the targeted cell.
About PTCL
Although there are clinical development programs ongoing with CAR T-cells for CD19+ cell hematological malignancies, CD4+ peripheral T-cell lymphomas (PTCLs) have not been targeted by a CAR therapy in a human trial. PTCLs account for 10–15 percent of all non-Hodgkin’s lymphomas (NHLs) and are more difficult to treat in comparison to B-cell NHLs.
Furthermore, and with few exceptions, T-cell NHLs have poorer outcomes, lower response rates, shorter times to progression, and shorter median survival in comparison to B-cell NHLs. As a result, the standard of care for PTCLs is not well-established and the only potential curative regimen is bone marrow transplant (BMT).
However, not only is BMT poorly tolerated, but is not an option for a significant subset of patients with resistant disease. This leaves many patients with no curative options.
About CD4CAR
CD4CAR is in development for CD4+ T-cell malignancies. The novel CD4-specific chimeric antigen receptor engineered T-cells are properly-matched allogeneic human T-cells engineered to express an anti-CD4scFV antibody domain. An initial Phase I clinical study is being planned through collaboration between iCell Gene Therapeutics, the National Institutes of Health, Indiana Clinical and Translational Sciences Institute, Stony Brook Hospital and the Blood and Marrow Transplantation Division and the Clinical Trial Research Unit at James Graham Brown Cancer Center at University of Louisville.
About iCell Gene Therapeutics
iCell Gene Therapeutics is focused on developing CAR T and NK cells that target and destroy multiple types of cancer. The primary focus is to treat and cure malignancies that have very poor prognoses and few available curative treatment options. The goal is to eradicate these devastating diseases, and to offer patients with resistant cancer a chance at a cure. Diseases covered by the company’s proprietary CAR technologies include B and T cell lymphoma and leukemia, myeloproliferative neoplasms, myeloid dysplastic syndrome (MDS), acute myeloid leukemia (AML), multiple myeloma (MM), non-hematological (non-blood) cancers and autoimmune disorders. For more information, visit www.icellgene.com.
OUCH! Why does stuff hurt? Find out at Beer with a Scientist, August 17
At this month’s Beer with a Scientist, Kristofer Rau, Ph.D., researcher at the University of Louisville School of Medicine, will discuss the neurobiology of why we feel pain. He’ll give an introduction to the neuroanatomy involved in pain processing and explain why the “funny bone” hurts so often, why we get ice cream headaches, why amputees feel pain in a lost limb and other painful topics.
Rau is a senior research scientist in the UofL Department of Anesthesiology and a member of the Louisville Chapter of the Society for Neuroscience. His work focuses on the neurobiology of pain and the electrophysiological and molecular changes that occur following tissue injury and spinal cord trauma.
The program begins at 8 p.m. on Wednesday, August 17 at Against the Grain Brewery, 401 E. Main St. A 30-minute presentation will be followed by an informal Q&A session.
The Beer with a Scientist program began in 2014 and is the brainchild of UofL cancer researcher Levi Beverly, Ph.D. Once a month, the public is invited to enjoy exactly what the title promises: beer and science.
Admission is free. Purchase of beer, other beverages or menu items is not required but is encouraged.
Organizers add that they also encourage Beer with a Scientist patrons to drink responsibly.
For more information and to suggest future Beer with a Scientist topics, follow Louisville Underground Science on Facebook.
Kristofer Rau, Ph.D.
UPCOMING BEER WITH A SCIENTIST EVENTS: Andrea Behrman, Ph.D., UofL Department of Neurological Surgery, September 14.
Beer with a Scientist founder, Levi Beverly, Ph.D., will speak at the event during Research!Louisville, October 12.
Annual UofL lecture will examine genetic-based precision medicine
“Sir William Osler and Modern Genetic-Based Precision Medicine” will be the topic of the 2016 Leonard Leight Lecture at the University of Louisville.
Ali J. Marian, M.D., will speak at noon, Wednesday, Oct. 5, at the 16th Floor Conference Center of the Rudd Heart and Lung Center, 201 Abraham Flexner Way. Admission is free. Marian is the George and Mary Josephine Hamman Foundation Distinguished Professor in Cardiovascular Research and the director of the Center for Cardiovascular Genetic Research at The Brown Foundation Institute for Molecular Medicine, University of Texas Health Science Center at Houston.
The Leonard Leight Lecture is presented annually by the Division of Cardiovascular Medicine in the Department of Medicine at the University of Louisville School of Medicine. For 30 years until 1996, Leight was a practicing cardiologist in Louisville and played a major role in developing cardiology services and bringing innovative treatment modalities in heart disease to Louisville.
The Leonard Leight Lecture series was established in 1994 and is made possible by gifts from Dr. and Mrs. Kurt Ackermann and Medical Center Cardiologists to the Jewish Hospital & St. Mary’s Foundation.
Regarded as the “Father of Modern Medicine,” Sir William Osler was a Canadian physician and in 1889, became founding physician-in-chief of Johns Hopkins Hospital in Baltimore. He later was a founding professor of Johns Hopkins School of Medicine, created the first residency program for specialty training of physicians and was the first to bring medical students out of the lecture hall for bedside clinical training.
Osler was known to have recognized the differences in the way disease manifests itself in each patient. “Variability is the law of life,” he said, “and as no two faces are the same, so no two bodies are alike, and no two individuals react alike and behave alike under the abnormal conditions which we know as disease.”
This recognition of the variability of patients’ reaction to disease is at the heart of today’s genetic-based precision medicine, and Marian will examine how Osler’s observations can provide insight in 21st Century medicine.
About Ali J. Marian, M.D.
Recognized internationally for his research achievements and expertise in genetics of cardiomyopathies, Marian earned his M.D in 1981 from Tehran University in Iran. He completed post-doctoral training at Cook County Hospital in Chicago in 1988 and at Baylor College of Medicine in Houston through the American Heart Association-Bugher Foundation Fellowship in 1991. He was appointed to the faculty at Baylor College of Medicine in 1992, and joined The Brown Foundation Institute of Molecular Medicine in 2006.
A past recipient of both the American Heart Association’s Established Investigator Award and the Burroughs Wellcome Fund’s Clinician-Scientist Award in Translational Research, Marian has served on the editorial boards of Circulation, Circulation Research, Journal of The American College of Cardiology and Genetics in Current Atherosclerosis Reports, among others, and has been lead or co-author of more than 100 manuscripts in peer-reviewed journals. He is actively involved with NIH grant reviews and has been a member of review committees on several panels and study sections.
Barry Kerzin, M.D., advocate for physician compassion, interviewed on "UofL Today with Mark Hebert"
Barry Kerzin, M.D., personal physician to the Dalai Lama, is featured on the "UofL Today with Mark Hebert" radio broadcast set for Monday, August 8, at 6 p.m. on 93.9 FM The Ville.
Kerzin, who was the keynote speaker at this year's UofL White Coat Ceremony on July 24, talked with Hebert about his life, his visit to Louisville, and the importance of training doctors to avoid burnout and retain their sense of empathy.
Hebert hosts two weekly 30-minute radio broadcasts focusing on research, programs, successful students and insights from UofL’s faculty experts which run on Monday and Tuesday during drive time on 93.9 FM. Listen to upcoming and past programs at https://soundcloud.com/uofl.
In the Tuesday, August 9, program, Ruth Carrico, Ph.D., of UofL's Global Health Initiative, talks about the spread of Zika virus, and MD Anderson surgeon Raymond Sawaya, M.D., who was in Louisville for the neuro-oncology symposium July 8, discusses surgical treatment for primary glioma. That program will air August 9 at 6 p.m. on 93.9 FM The Ville. The programs are repeated on Saturday and Sunday mornings.
Underrepresented undergraduate students gain medical research experience in summer program
This summer, Kayla Massey is using an infrared spectrometer at the University of Louisville to determine how the structure of a lipid called meibum found in the eyelid affects tears in the eye. Massey, who will be a junior at Howard University this fall, is spending the summer in Louisville to gain experience working in a research lab that will help her when she applies to a post-graduate program.
“I’ve done research in biology before, but this is centered around the lipids in the eye so it is a lot more about organic chemistry. It is good for me because I had never done any chemistry research before,” Massey said.
Massey is one of 10 students participating in the Summer Undergraduate Experiences in Biomedical Research program, directed by Irving Joshua, Ph.D., chair of the Department of Physiology at UofL. The program, supported by a grant from the National Institutes of Health, allows students who are economically disadvantaged, the first in their family to attend college, underrepresented minorities or from underserved areas to spend 10 weeks working in research labs with faculty mentors in areas such as diabetes, kidney disease and heart disease.
“Our goal is to get more underrepresented minority and disadvantaged students involved in research, doctoral programs and medicine. This experience will give them exposure to clinical research that can help them in their careers,” Joshua said.
The Association of American Medical Colleges and the National Academy of Medicine support the idea that a diverse workforce in health care and biomedical research will serve to reduce health disparities in the United States.
Massey, a biology major who hopes to attend medical school and become a surgeon, is being mentored at UofL by Douglas Borchman, Ph.D., professor in the Department of Ophthalmology & Visual Sciences. His research focuses on dry eye and cataracts related to diabetes.
“I am interested in diabetes and high blood pressure. Dr. Borchman is doing work with the effects that glucose has on lenses,” Massey said. “I think it’s opened my eyes to more about science and medical research in general.”
Borchman hopes to encourage Massey and other students in the program to pursue graduate study or medicine by engaging them in the research experience.
“The program can lead to them going on to grad school, which is great,” Borchman said. “I enjoy seeing the spark in the students, showing them that research is fun and not tedious. I give them responsibility and a long leash but don’t let them stray too far. They are young and enthusiastic and it is fabulous.”
One of Borchman’s former summer undergraduate mentees, Samiyyah Sledge, is now a Ph.D. student at UofL in physiology and biophysics with a concentration on the eye. Sledge said her experience as a summer undergraduate in 2014 piqued her interest in this area of research and introduced her to opportunities in graduate programs.
“This lab fostered and developed my love for the eye and for research in general,” Sledge said. “The exposure and experiences I gained here influenced my decision to join the physiology Ph.D. program. In addition, Dr. Borchman himself has been a great and supportive mentor to me.”
Maura Fordham, another program participant this summer, will attend UofL this fall as a biology major, after transferring from Jefferson Community and Technical College. Fordham is working in the lab of Utpal Sen, Ph.D., associate professor in the Department of Physiology, whose research focuses on kidney disease.
“We are looking into diabetic nephropathy regulating Micro RNA 194 through the synthetic drug GYY 4137,” Fordham said. “It’s taught me technique and how you handle yourself in a lab. I've gained an incredible amount of knowledge this summer from everyone in Dr. Sen's lab. I know this experience will help me as I continue as an undergrad and eventually as a medical student.”
Sen said the summer students he mentors often are successful in applying to post-graduate programs.
“I want to get summer students in as undergraduates to get them interested in a research career that is both fun and challenging, yet rewarding,” Sen said. “Some go on to do a master’s or PhD program, and many of them are getting into medical school. It is a good basic research experience for them. They get used to the faculty and the programs our university offers and it helps them get into those programs. When these students are successful in their future careers, everyone benefits – the department, the university, the candidate and the mentor. We need more of these young minds to get involved in active biomedical research to advance the field for human well-being.”
Joshua said students typically participate following their sophomore or junior year of college and are paired with investigators working in areas of interest to them. TheprogramatUofLhas been supported by a grant from the National Heart Blood and Lung Institute, part of the National Institutes of Health, since 2006 and is open to students attending colleges in and outside of Kentucky. Student selection is based on their grades, an essay describing their interest in scientific and biomedical research, and how well their areas of interest mesh with available mentors at UofL.
To conclude the program, the students will give a five to 10-minute presentation of their research and present posters along with other summer research program participants on Wednesday, August 3, from noon until 3 p.m. in the Kosair Charities Clinical and Translational Research Building, 505 S. Hancock St.
UofL medical school husband and wife alumni return to practice with ULP
Nurse Practitioner Christine Kerr, left, confers with Drs. Chris and Connie Angellis in their clinic at the University of Louisville Physicians Outpatient Center. The Anggelises, both UofL School of Medicine alumni, recently returned to UofL to practice.
Thirty-four years after they met as students at the UofL School of Medicine, cardiologists Drs. Chris and Connie Anggelis have joined University of Louisville Physicians and the school’s faculty.
They started seeing patients in June at the UofL Physicians Health Care Outpatient Center.
“I’m very excited about returning to the university,” said Connie Anggelis. “We went to medical school here, and we’ve been practicing in Louisville since. We toured the medical school during a class reunion, and it brought back great memories. We’ve been talking about doing this for a number of years.”
Chris said their return to the university “allows us to maintain our focus on patient care while giving something back to the community." He said he enjoys teaching young doctors, “and hopefully some of them will stay in this community.”
For he and Connie, patient care is paramount. “It’s more about quality rather than the number of patients you see,” said Connie. “I think doctors need to be able to spend adequate time with their patients. It allows us to educate them about cardiac issues. We also want to teach students to always put the patient first.”
Chris said their goal is to be available and responsive to patients’ needs. “We’re going to have multiple offices in different areas to accommodate them,” he said.
In addition to downtown at the UofL Physicians Health Care Outpatient Center, they will be seeing patients at offices in eastern Jefferson County (Jewish East and Jewish Northeast) and in Hillview in Bullitt County, where they have practiced in the past. They will also see patients at Jewish Hospital downtown.
 “If a patient needs to be seen, we will see them when the referring doctor wants them seen,” Chris said.
“If a patient needs to be seen, we will see them when the referring doctor wants them seen,” Chris said.
Chris focuses on interventional cardiology and Connie on non-invasive cardiology, and both are passionate about preventive care, guiding patients on how to achieve health goals and do the little things to prevent big problems with their hearts later.
“An ounce of prevention can go a long way,” Connie said. “You would much rather see me before an event occurs, rather than after. I do my best to educate my patients.”
She said the combination of heart disease and stroke is the leading cause of death in Kentucky, and better education and prevention is needed.
“We have a long way to go in respect to prevention in Kentucky,” she said. “It’s about getting people to want to change their lifestyle. Preventive care can improve the quantity and quality of life.”
 Medicine in the family
Medicine in the family
After meeting as students at the UofL School of Medicine, Chris and Connie double-matched for their residencies in internal medicine at Wake Forest and for fellowships in cardiovascular disease at Emory.
After their training was finished in 1990, they returned to Louisville. For them, it was returning home. But after 25 years in private practice together, they felt it was time to return to UofL.
“We received our medical education from UofL, and raised our children in this community,” Chris said.
All three of the Anggelis’ children are in health care: Their son, Nick, just finished dental school at UofL; one daughter, Lauren, is in the doctoral program for clinical neuropsychology at UofL; and another daughter, Emily, is in medical school at the University of Kentucky.
“We love our state and it is so nice to be back at UofL, where it all began for us,” said Connie.
UofL dermatology chief elected to national committee
Jeffrey P. Callen, M.D., chief of the Division of Dermatology at the University of Louisville School of Medicine, has been elected to serve on the Accreditation Review Committee (ARC) of the Accreditation Council of Continuing Medical Education (ACCME). His two-year term begins Dec. 1, 2016.
The ACCME is a nonprofit organization based in Chicago that is responsible for accrediting institutions throughout the United States that offer continuing medical education (CME). Accreditation decisions are determined through a review by two ACCME committees: first, the Accreditation Review Committee, and second, the Decision Committee of the Board of Directors. All accreditation decisions are then ratified by the ACCME’s Board of Directors.
All physicians are required to earn CME credit in order to maintain their license to practice. In Kentucky, all physicians who maintain an active Kentucky medical or osteopathic license are required to complete 60 hours of CME every three years.
A Chicago native, Callen earned his undergraduate degree from the University of Wisconsin in Madison before earning his medical degree from the University of Michigan, where he also performed residencies in internal medicine and dermatology.
In 1977, Callen joined the faculty at the University of Louisville, attaining the rank of professor in 1988 and being appointed as chief of the Division of Dermatology the same year. He served on the Board of Directors of the Dermatology Foundation from 1983-88; the American Academy of Dermatology from 1994-98 and 2003-04 as vice president; and the Association of Professors of Dermatology Inc. since 2003. He was the chair of the Council on Education of the American Academy of Dermatology 2003-07. He has been a member of the board of the American Board of Dermatology and the American Dermatological Association. He is a past president of the Medical Dermatology Society and was awarded the society’s Lifetime Achievement Award in 2011. In 2009 Callen received the Thomas Pearson, Ph.D. Education Award from the American Academy of Dermatology. This September he will assume the Presidency of the Association of Professors of Dermatology.
Callen is the author or co-author of 84 original articles, 181 case reports, 149 review articles, 50 editorials, 15 books, 276 book chapters and 165 abstracts. He has served as editor or deputy editor of the Archives of Dermatology, Journal Watch Dermatology and the Dermatology Section of UpToDate. He is currently the Associate editor of JAMA Dermatology. His book, Dermatologic Signs of Systemic Disease, now in its fifth edition, was just published.
Locally, Callen has served on the boards of the Jewish Community Center, Jewish Family and Vocational Services, Actors Theatre of Louisville, the Kentucky Arts and Crafts Foundation and the Speed Art Museum.
UofL faculty and staff introduce at-risk youth to careers in health care
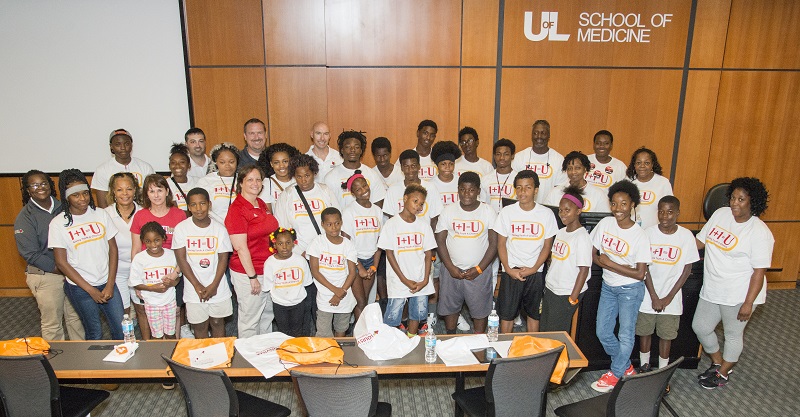
Twenty-six students from the Shawnee neighborhood who are participating in the 1+1=U Summer Youth Enrichment Program visited the University of Louisville Health Sciences Center Wednesday, July 20, to learn about sports medicine, healthy habits and steps to a career in health care.
Health-care professionals and faculty members from the School of Medicine and College of Education and Human Development talked with the students, from 12 to 17 years old, about the paths they took to careers as an athletic trainer, physical therapist, physician, teacher and exercise physiologist. In addition, they offered tips on recovering from sports injuries and healthy eating and activity. The visit was organized to introduce the students to opportunities for careers in health care.
1+1=U is a year-round mentoring program that targets students who have had academic and behavioral challenges in and out of the classroom. The program assists young men and women get in position to further their education beyond high school by boosting academic and personal achievement, sports achievement and parental and family involvement. The summer program is a two-week-long extension of that effort based at the Shawnee Arts and Cultural Community Center.
Brittney Richardson, M.D., a sports medicine fellow and board certified family physician at UofL and KentuckyOne Health, told the students about her journey to becoming a physician, a path she navigated despite the fact that no one in her family had been a health care professional.
“I want to show them that there are opportunities out there for them to succeed,” Richardson said. “I was connected along my way with the right people, but that doesn’t happen all the time. I can be that person for them to be connected with and I don’t think I have reached my goal until I have helped someone get to where I am.”
One of the students, Daihjae Tandy, said she was interested in the information about nutrition and concussions and definitely is planning to go to college. Although the high school junior is interested in art, she said she would consider a career in health care after hearing the presentation.
“I think it would be great. I even thought about it after hearing everything they do. It’s actually very wonderful for anybody,” Tandy said.
Margaret Dunbar-Demaree, founder and director of 1+1=U, began mentoring troubled students as a teacher at Central High School. Now retired from her teaching position, Demaree mentors and tutors students at the Shawnee Arts & Cultural Community Center and Bethel Baptist Church.
This is the third year the 1+1=U Summer Youth Enrichment Program students have visited the UofL HSC Campus. For more photos from the visit, click here.
 Brittney Richardson M.D.
Brittney Richardson M.D.
Parkinson’s Disease Buddy Program seeking participants
Individuals diagnosed with Parkinson’s Disease are invited to participate in the Parkinson’s Disease Buddy Program, which matches them with first-year University of Louisville medical students for a series of one-on-one meetings designed to benefit both students and the patients. Buddies will be paired for one calendar year beginning in September, meeting two to three hours a month and at special group events.
The PD Buddy program, the only one of its kind for Parkinson’s patients, was launched last summer as a partnership between UofL and the Parkinson Support Center of Kentuckiana. Twenty-five buddy pairs participated in the year-long program designed to give the patients social interaction and allow them to share their stories with the students, who in turn gained first-hand knowledge about living with a nervous system disorder. The program also serves to better educate students about Parkinson's, introduce students to research and career opportunities in neurology and movement disorders, and provide people with Parkinson's Disease the opportunity to interact more closely with the medical community.
Kathrin LaFaver, M.D., the Raymond Lee Lebby Chair for Parkinson’s Disease Research in the Department of Neurology at UofL and director of the Parkinson’s and Movement Disorders Clinic at UofL Physicians, said the exchanges give the students a deeper understanding of how patients cope with the disease. LaFaver also meets monthly with the students to provide additional medical information and inform the students about research and career opportunities in neurology and movement disorders.
Since this program is unique for Parkinson’s patients, LaFaver, along with Erika Branch, executive director of the Parkinson Support Center, and Denise Cumberland, Ph.D., assistant professor in the UofL College of Education and Human Development, will present findings from the first year of the PD Buddy Program at the World Parkinson Congress in Portland, Ore., in September.
The PD Buddy Program, also sponsored by KentuckyOne Health, is open to anyone diagnosed with Parkinson's Disease who has the time and interest to participate. In addition to one-on-one meetings with the students, several group activities will be planned over the course of the year. Patients must understand that this is an education program and that the medical students will not be able to give medical advice.
Interested individuals may call the UofL Physicians Movement Disorders Clinic at 502-582-7654, the Parkinson Support Center of Kentucky at 502-254-3388, or email a completed application form to outreach@parkinsoncenter.org prior to August 15. Application forms may be downloaded at https://www.uoflphysicians.com/sites/default/files/pdf-files/PD-Buddy-Patient-Sign-up.pdf.
Personal physician to the Dalai Lama speaks on compassion in medicine at UofL White Coat Ceremony
Barry Kerzin, M.D., personal physician to the Dalai Lama and founder of the Altruism in Medicine Institute, addressed the 156 members of the incoming class of the University of Louisville School of Medicine and guests at the school’s White Coat Ceremony on Sunday, July 24. Kerzin, an American trained physician and Buddhist monk, spoke to the students about cultivating and preserving the desire to help others.
“Compassion is the chief reason we all go into medicine,” Kerzin said prior to the event. “Research suggests at the third year of medical school, compassion in medical students decreases significantly. I'll address how to sustain our compassion through our training and out in the world practicing medicine.”
The ceremony welcomeed the class of 2020 to the UofL School of Medicine. The students each received a white coat, a gift from the Greater Louisville Medical Society, and a stethoscope, provided by an alumnus of the school through Stethoscopes for Students. The white coat symbolizes cleanliness, as well as the sense of compassion that inspires students to become physicians. At the ceremony, the students recited the Declaration of Geneva, promising to serve humanity and honor the traditions of the medical profession.
Kerzin, a California native, is a board-certified family medicine physician and an honorary professor at the University of Hong Kong School of Medicine. He is a former assistant professor of medicine at the University of Washington School of Medicine in Seattle. After traveling to India in the 1980s to help train Tibetan doctors in modern research methods, he studied Buddhism and meditation and ultimately was ordained as a Buddhist monk. Kerzin now provides medical care to the poor in India and serves as a personal physician to the Dalai Lama in addition to traveling around the world to teach about meditation and compassion. He founded the Altruism in Medicine Institute with the goal to bring more compassion into health care.
UofL School of Medicine White Coat Ceremony
Sunday, July 24, 3-5 p.m.
Louisville Downtown Marriott
280 W. Jefferson St., Louisville, Ky., 40202
Originally published July 20, 2016. Updated August 5, 2016.
Nominate an outstanding nurse for 3rd annual UofL Nightingale Awards in Nursing
University of Louisville School of Medicine faculty, staff, students, residents and alumni are invited to nominate outstanding nurses employed in Kentucky and Southern Indiana for the third-annual University of Louisville Florence Nightingale Awards in Nursing.
The awards honor exceptional nurses who have followed in the footsteps of Florence Nightingale, the founder of modern nursing.
Submit an essay of no more than 200 words about how a registered nurse meets at least one of the following categories:
- Impacted patients through excellent and compassionate nursing care;
- Improved health outcomes in a population or in the community;
- Elevated the nursing profession through teaching, research and/or policy development;
- Inspired others to consider nursing as a career.
People may nominate a nurse online. The nomination deadline is Sept. 8.
Winners will receive a cash prize and commemorative plaque at the Nightingale Awards dinner 5:30 to 8 p.m. Nov. 3 at the Mellwood Arts Center. Register to attend the dinner.
For more information, contact Karen Rose at karen.rose@louisville.edu or 502-852-5825.
UofL opens NIH-designated Alcohol Research Center
Alcohol abuse exacts a major toll on health and health costs in the United States and is the 3rd leading preventable cause of death. Researchers at the University of Louisville have received a nearly $8 million grant from the NIH that designates them as an NIAAA Alcohol Research Center.
The UofL Center is one of only 20 in the nation. It’s funding score for the grant was the best in the nation. It is the only center with a nutrition focus.
“We are going to take a unique focus into organ injury associated with alcohol use,” said Dr. Gregory C. Postel, interim executive vice president for health affairs at UofL. “Our researchers are going to examine the interactive role of nutrition and alcohol in the deleterious, as well as beneficial, effects of alcohol on the human body.”
Through four different projects, the research team led by Dr. Craig McClain, associate vice president for translational research and associate vice president for health affairs/research, has three specific aims:
- Facilitate interdisciplinary approaches and serve as a regional/national resource for the study of nutrition and alcohol-induced organ injury;
- Provide a robust pilot project program and comprehensive education and research training in order to develop the next generation of alcohol investigators; and
- Develop potential therapeutic targets/interventions for alcohol induced organ injury based on the mechanistic research of the center and translate knowledge/interventions to the community.
“This funding will allow us to look at the problems that alcohol abuse causes, as well as the potential benefits of alcohol,” McClain said. “Our focus on dietary nutrition and abuse is unique. For example, only a small proportion of people who abuse alcohol will develop liver disease. We believe that the type of dietary fat intake is critical in the development of alcohol-induced organ injury.”
To find answers, the center will initially focus on four projects.
Project 1 will evaluate the role of dietary unsaturated fat in the development/progression of alcoholic liver disease.
Project 2 will evaluate alcohol-induced alterations in the gut-liver axis. Researchers will examine the role of histone deacetylases (HDACs) in both the intestine and liver in alcohol-induced gut-barrier dysfunction and steatohepatitis and the role of probiotics and dietary HDAC inhibitors in preventing/treating experimental ALD.
Project 3 will determine mechanisms by which maternal alcohol consumption causes mental retardation in the offspring. Researchers will evaluate epigenetic mechanisms by which alcohol induces apoptosis and teratogenesis, and by which the nutraceutical, sulforaphane, provides epigenetic protection.
Project 4 will evaluate mechanisms by which alcohol causes increased susceptibility to acute lung injury. They postulate that chronic alcohol intake triggers extracellular matrix remodeling resulting in “repavement” of lung tissue with a proinflammatory extracelluar matrix and that this process can be modulated by dietary intervention.
“Our studies are designed to look at a number of organ systems, not just the liver,” McClain said. Additionally, we are very interested in gaining a better understanding of the role alcohol may play during fetal development and the mechanisms associated with fetal alcohol syndrome.”
The research team spans 13 departments at UofL in six schools/colleges.
“One of the keys to developing the breadth of information we hope to achieve is bringing together people with expertise in areas that often are not combined,” McClain said. “It is important that we look at these issues from a broad perspective if we are to examine the overall impacts of alcohol.”
Is it better to be lucky or good? Paula Bates, Ph.D., talks about serendipity in scientific discovery at the next Beer with a Scientist, July 20
Scientists have made some amazing discoveries by accident, including penicillin, the microwave oven and Viagra. Of course, the scientists needed to have specific knowledge in order to recognize their discoveries.
At this month’s Beer with a Scientist, Paula Bates, Ph.D., will talk about the role serendipity has played in many scientific discoveries as well as her own career as a scientist. Bates, associate professor at the University of Louisville Department of Medicine and researcher at the James Graham Brown Cancer Center, “accidentally” discovered a new cancer therapeutic that has been since used in patient clinical trials.
In her research, Bates focuses on identifying and characterizing novel cancer therapeutics. Her work has led to the clinical trials of a ‘first in humans’ therapeutic called AS1411, a DNA aptamer, which was, in fact, a serendipitous discovery. AS1411 folds into a G-quadruplex structure that binds to nucleolin (a protein present at high levels on the surface of cancer cells) and can kill cancer cells without harming non-malignant cells. She and her colleagues are now also using AS1411 to guide various nanoparticles to cancer cells, which could lead to better methods for cancer detection and therapy.
Bates also is principal investigator for University of Louisville ExCITE, an NIH Research Evaluation and Commercialization Hub, created to facilitate the translation of biomedical innovations into commercial products that improve patient care and enhance health.
The program begins at 8 p.m. on Wednesday, July 20 at Against the Grain Brewery, 401 E. Main St. A 30-minute presentation will be followed by an informal Q&A session.
The Beer with a Scientist program began in 2014 and is the brainchild of UofL cancer researcher Levi Beverly, Ph.D. Once a month, the public is invited to enjoy exactly what the title promises: beer and science.
Admission is free. Purchase of beer, other beverages or menu items is not required but is encouraged.
Organizers add that they also encourage Beer with a Scientist patrons to drink responsibly.
For more information and to suggest future Beer with a Scientist topics, follow Louisville Underground Science on Facebook.
COMING NEXT MONTH: On August 17, Kristofer Rau, Ph.D., researcher in the UofL Department of Anesthesiology, will discuss the neurobiology of why we hurt. He’ll explain why the “funny bone” hurts so often, the placebo effect, why amputees feel pain in a lost limb and other painful topics.
Behrman, Harkema to present latest developments in therapy at international conference
Researchers in the University of Louisville Department of Neurological Surgery will share their recent developments in therapies for children and adults with neurological conditions at IV STEP, an international conference intended to foster, guide and affect neurologic physical therapy practice over the next decade. Andrea Behrman, Ph.D., P.T., and Susan Harkema, Ph.D., professors at UofL, along with Elizabeth Ardolino, Ph.D., P.T., assistant professor at the University of St. Augustine, will present “Activity-dependent Plasticity for Neuromuscular Recovery: Use of Classifications to Drive Therapies and Outcomes,” on Friday, July 15, at the IV STEP Conference in Columbus, Ohio.
In their presentation, the researchers will discuss how therapies aimed at recovery and improved function after neurological injury or disease can be designed based on key scientific evidence of the ability of the central nervous system to change through physical activity, a process known as activity-dependent plasticity. They will discuss how evidence for this process can be used in the treatment of children with chronic spinal cord injury. The sensorimotor experience of typical childhood development, current rehabilitation after pediatric SCI, and activity-based therapies will be explored as a basis for different outcomes and expectations.
To assist in the development of these novel therapies, the team will introduce the Neuromuscular Recovery Scale and the Pediatric Neuromuscular Recovery Scale, tools for assessing the neuromuscular capacity of adults and children to perform functional tasks without compensation from behavioral strategies, equipment or physical assistance. The scale can be used to classify capacity and track recovery in individuals with neurologic injury or disorders.
“One aim of this assessment is to capture incremental gains in motor function. Assessing ‘how’ the movement is performed also addresses the quality of the movement, which distinguishes this measure from many other pediatric instruments typically in use,” Behrman said.
With funding from the Department of Defense and the Craig H. Neilsen Foundation, the group has established the validity, reliability, responsiveness and other properties of the scale, which will pave the way for it to be incorporated into clinical practice and research. Other aspects of the research are supported by the Leona M. and Harry B. Helmsley Charitable Trust, the Christopher and Dana Reeve Foundation and Kosair Charities.
The IV STEP conference, sponsored by the Pediatric and Neurology Sections of the American Physical Therapy Association (APTA), is designed to explore new theory and research evidence related to movement science and to translate this theory and evidence into physical therapy practice. The six-day program will include 33 invited speakers, 13 video case presentations and 100 peer reviewed poster presentations for approximately 700 clinicians, educators, and researchers from around the United States and abroad.
It is only the fourth such conference to be held in 50 years. The first, NUSTEP, was held in 1966 and the second, II STEP, in 1990. At III STEP, held at the University of Utah in June 2005, Behrman presented information on her research in using locomotor therapy, “Locomotor recovery after SCI: From basic science to clinical practice.”
In addition to the invited plenary presentation by Behrman and Harkema, five research teams from Frazier Rehabilitation Center, a part of Kentucky One Health, and the University of Louisville will be presenting posters.
Behrman is a professor in the UofL Department of Neurological Surgery and director of the Kosair Charities Center for Pediatric NeuroRecovery. Her research focus is to develop and test therapeutic interventions promoting recovery after spinal cord injury in children and adults capitalizing on activity-dependent neuroplasticity and an understanding of the neurobiology of walking and motor control. Her research has demonstrated improvements in trunk control in children in particular.
Harkema is a professor in the UofL Department of Neurological Surgery and associate scientific director of the UofL Kentucky Spinal Cord Injury Research Center. Harkema’s research in epidural stimulation in adults shows promise in helping individuals recover function following complete spinal cord injury.
The University of Louisville is an academic sponsor of the IV STEP Conference.
 Facebook
Facebook Twitter
Twitter Linkedin
Linkedin