News
UofL study shows heart transplant access, outcomes for Black patients improved significantly since 1987
Jaimin Trivedi, assistant professor and director of clinical research and bioinformatics in the UofL Department of Cardiovascular and Thoracic Surgery
Researchers at the University of Louisville analyzed data for heart transplants from 1987 to 2019 to better understand equity in access to heart transplant for adult Black and white patients and those of other races, comparing percentages of patients who were placed on the transplant list and those actually transplanted over time. They found that access to transplants for Black patients has improved significantly over the study period, both in the percentage of patients listed for transplant and the percentage of transplants performed.
Jaimin Trivedi, assistant professor and director of clinical research and bioinformatics in the UofL Department of Cardiovascular and Thoracic Surgery, was lead author on an article published in PLOS ONE last month detailing the findings.
Trivedi and his colleagues in the department used data from the United Network for Organ Sharing (UNOS) database to analyze changes in the percentage of heart transplants for Black, white and patients of another race since 1987, when the database was established. They analyzed de-identified records for a total of 105,266 adults listed in the database for heart transplants from 1987 through 2020 by Black, white or another race, and the 67,824 patients from the list who received a heart transplant.
The proportion of Black patients on the UNOS heart transplant list increased form 7% in 1987 to 25% in 2019 and those who received transplants increased from 5% in 1987 to 26% in 2019.
According to 2020 U.S. Census data, 14.2% of the U.S. population is Black or African American alone or in combination with another race.
“Black patients historically have had poorer access to heart transplants, evident in our study as fewer patients listed for transplant and fewer patients actually receiving the transplant,” Trivedi said. “But, as the general health care of heart transplant patients improved over the years and the knowledge of racial disparities came into light, all these things came together and eventually the proportion of Black patients listed increased over time.”
While the numbers indicate parity among patients of different races, Trivedi said an analysis of equity must also consider the increased risk for heart disease among Black patients.
“The Black population is at higher risk of cardiac disease based on the CDC data, so that means there are more Black patients likely to have heart failure and they are more likely to require a heart transplant,” Trivedi said. “If we are just looking at two numbers in the proportion of patients transplanted right now, it's improved, but we have to look at it from the perspective of how prevalent heart disease is in the Black community and then how many of them are getting a transplant. So more research has to be done before you can meaningfully say whether there is equity in access to heart transplants.”
The researchers examined three-year survival of heart transplant patients. Post-transplant outcomes improved for all patients over the study period due to better post-transplant care, more rapid treatment of transplant rejection and other factors. Outcomes also improved for Black patients, which are reaching levels comparable to white and other patients in recent years.
“There has been a general improvement in transplant survival outcomes across the races. Black patients tended to do slightly more poorly than white patients, but when we look at more recent data over the past five or six years, we have seen that Black patient survival also has been improving and it is reaching par.”
Another factor affecting post-transplant survival is access to quality health insurance. With this in mind, the researchers compared data for individuals with private insurance with those who had Medicare or Medicaid, information that was included in the database since 1994.
They found that post-transplant survival for Medicare and Medicaid patients improved over time but remained marginally below that of private insurance patients. The improvement in survival of Black patients was seen through all insurance classes over time, particularly since 2012, which Trivedi said could be multifactorial but also partially due to reliable insurance coverage after the application of the Affordable Care Act.
Real-life Wonder Woman: UofL School of Medicine dean shares her serendipitous journey into medicine and science
Toni M. Ganzel, MD, MBA, dean of the UofL School of Medicine, joined UofL in 1983 as an assistant professor of otolaryngology. In 2001 she was named associate dean for student affairs and in 2003, senior associate dean for students and academic affairs. In 2013, Ganzel became the first female to be appointed dean of the UofL School of Medicine. In 2020, she was appointed vice president for academic medical affairs.
In honor of International Day of Women and Girls in Science, UofL News talked with Ganzel about her journey into medicine and science.
UofL News: Tell us about your journey into medicine.
Toni Ganzel: I didn’t grow up with the goal of going into medicine. In fact, my first life aspiration that I can remember was wanting to be Wonder Woman because I fancied the idea of flying around the world and saving people. And I also was fond of the red high heel boots and the outfit.
The sixth grade was a pivotal time in deciding what career to pursue because it was then that I fell in love with science. Science mesmerized me – especially biology – and I was fascinated by how the body worked. So, what I thought I wanted to do then was to be a high school biology teacher. My other two areas of avid interest in middle school and high school were cheerleading and student government. This led to deciding my dream job was to be a high school biology teacher, cheerleading coach and student government sponsor.
But when I got to college and took more advanced sciences, I realized that teaching high school biology may not challenge me enough and I considered medical research instead. A friend suggested I take the MCAT and go into medicine, which is something I hadn’t considered. I took the advice, took the MCAT, applied to medical school, got accepted and have never looked back. I can’t imagine any other profession bringing me the joy and fulfillment that being a pediatric ENT surgeon and medical educator did. And for the past 10 years, being the dean is equally rewarding and has been an amazing opportunity to help shape the future of the institution and to work every day with talented students, residents, faculty and staff.
My path to medicine was almost serendipitous and I tell students today that path doesn’t necessarily work for everyone, that more intentionality is needed. As I take a step back and think about how to find the sweet spot of a career, it’s marrying your goals and passions and seeking opportunities to bring those two things together. I loved science, loved helping people and loved learning. Medicine was the perfect marriage.
UofL News: What are some of the biggest challenges you have faced in your career?
Ganzel: The biggest challenge was and is the time commitment. The time challenge started in medical school and has continued ever since. While I try and make a conscious effort to balance work and family, it’s always a struggle.
UofL News: What has been your most rewarding moment in medicine?
Ganzel: Rather than a single moment, it has been a series of moments and it’s on really two tiers – thinking about being a physician versus thinking about being dean. My field of training was ENT surgery and specifically pediatric ENT, so I did lots of tonsils and tubes and airway work and every one of those was so rewarding. I probably did 15,000 tubes and 10,000 tonsillectomies and adenoidectomies, and never got bored. Children had repeated ear infections and hearing loss and they nearly always got better when they got tubes. Children snored and obstructed at night from large tonsils and adenoids, and they nearly always got better when they had their tonsils and adenoids out. It was so gratifying to be able to improve the quality of life of not just the children, but their families as well.
Then, when I think about being the dean, and previously the student affairs dean, it has been so rewarding to touch students’ lives and watch their own professional growth and development. I had the joy of teaching students and then watching them develop incredibly successful careers as physicians and as leaders. Now, as dean, I not only get to work with students and trainees, but with incredible faculty and staff and fantastic colleagues and leaders across the institution and across the country. I am very blessed to be able to do work that I love.
UofL News: What would you tell other women interested in joining the medical field?
Ganzel: If you love science, if you love learning, if you love helping people, it is a wonderful field. However, you also need to be mindful of the time commitment because it’s a big one. And while work-life balance will be a challenge, it is a profession that will bring you great joy, humility and gratification.
UofL News: What is one thing you wish you could tell your past self during medical school?
Ganzel: I would tell myself to remember that medical school is not a destination, but it’s part of a career journey. And on those days that feel daunting, to keep the long view in mind and take time to remember why I chose this life career.
UofL News: What do you like to do outside of work?
Ganzel: I love spending time with my family and my dogs. I like to exercise, my husband and I like to travel and we love mountain sports of hiking, skiing and mountain biking. And while we like to be active, we also enjoy reading and relaxing as well.
UofL News: What is your hope for the future of medicine?
Ganzel: That this pandemic gets over. It has been a nightmare. But I’m proud of the way that we have risen to the occasion and the resilience that we have shown.
Another hope for the future of medicine is that our increased focus and commitment around health equity will result in better health care and better health for all. Finally, I hope that our research discoveries will continue to lead to new cures and healthier people.
New York man with paralysis stands 39 years after injury thanks to UofL’s spinal cord research
Nearly four decades after Henry Stifel’s spinal cord injury – and after following spinal cord injury research as a philanthropist for more than three – the opportunity came for him to participate in epidural stimulation research at the University of Louisville.
On one level, it was a dream come true, but he had to think carefully about it before accepting.
Before he enrolled, he took stock of his goals. Did he have expectations about what he might gain? Was he doing it only for himself? Finally, he was about to get married and it would require relocating to Louisville from his home in New York City for an extended period of time.
Ultimately, he decided his participation could benefit other older SCI patients and those longer post-injury – he was 55 years old and 39 years post injury. The possibility that he could benefit personally was a bonus – but an exciting one.
“My wife said I would be regretting it for the rest of my life if I didn’t do it,” Stifel said. “I admit I was like a kid in a candy shop – I wanted that candy! But I knew I would have to work extra hard.”
From philanthropist to participant
Stifel was 17 years old in 1982 when an auto accident left him paralyzed, unable to walk or use his hands. With support from his family and community, he got on with life, graduating from high school, then college with a degree in finance and pursuing a career on Wall Street.
Hoping to change the trajectory of spinal cord injury research, dubbed the “graveyard of neuroscience,” Stifel and his father started a foundation to raise money and fund research that would give hope for recovery to people with spinal cord injuries. That foundation eventually merged with the American Paralysis Association and later with what now is known as the Christopher and Dana Reeve Foundation, supporting research and advocacy for individuals with spinal cord injury (SCI).
As a board member of the foundation throughout its history, Stifel followed the work of SCI researchers, particularly UofL professor Susan Harkema and Kentucky Spinal Cord Injury Research Center. He was impressed with the progress they made using implanted epidural stimulators, from Rob Summers, the first individual implanted with a stimulator for SCI research, to additional participants who experienced voluntary movement, improved cardiovascular function, the ability to stand and improved bowel, bladder and sexual function. Some even took steps because of the implant and specialized therapy developed by the UofL team.
Stifel, now in his 50s, was gratified to see this progress and support the work through the foundation, including “The Big Idea,” a 36-participant study of the benefits of epidural stimulation funded by the Reeve Foundation and led by Harkema. The previous participants were younger and had a shorter length of time since their injury. Although he had been to Louisville to participate in other studies, Stifel believed that because it had been nearly 40 years since his injury, it was unlikely he would be able to participate in the epidural stimulation studies.
Then in 2018, Stifel got a call to participate in The Big Idea. Since his deficits were stable, which gave the researchers a solid starting point to document any gains or changes he might experience, he qualified.
When he arrived in Louisville for the study in 2020, he knew that nothing was guaranteed.
“I understood that you need to go in with zero expectations,” Stifel said. “You can only have expectations if the therapy is proven, but it is still being tested. My goal was to be involved and represent others who are injured as long as me. I wanted to help the research progress.”
Blood pressure regulation and stand training
Stifel’s overall health had remained relatively stable in the years since his injury, without many of the comorbidities people with severe SCI often experience. The one side effect he did have was chronic low blood pressure.
“My blood pressure was typically 80/50, which can be debilitating,” he said. “I became used to it, but it is not a healthy way to live. When I was giving a presentation or having a conversation, I would find myself distracted.”
Once enrolled in the study, Stifel underwent preliminary assessments followed by the surgery to implant the electrode on his spine and the epidural stimulator in his abdomen. Then the researchers did a series of mapping sessions in which the stimulator was tested for each of the areas being studied: voluntary leg movement, trunk control and cardiovascular function.
Stifel was randomized into a cardiovascular arm of the study, which required that he monitor his blood pressure every 15 minutes for six hours a day, keeping his systolic blood pressure between 110 and 120. If it dropped below that, he was to adjust the stimulator to regain that level.
Those sessions brought significant improvement for Stifel.
“I didn’t realize how poorly I felt until it was fixed. I guess you have to feel bad to realize what good feels like,” he said. “When my blood pressure maintains a healthy level, it is like a breath of fresh air. My ability to engage, be proactive and live life is so much easier.”
Now, even when he turns off the stimulator, his blood pressure remains above its previous levels for several hours.
Stifel’s study protocol also included 160 two-hour stand training sessions in the lab at UofL Health – Frazier Rehab Institute. Every weekday, he would stand upright in a standing frame with trainers supporting his back, chest and each knee. These sessions were to help Stifel gain strength and independence.
“At the end of the sessions, I could consistently stand for 10-to-16 minutes without knee support,” Stifel said. “The epidural stimulator is more intense and effective than anything else I have experienced.”
Moving the needle
Stifel’s time since injury is the longest of any of the participants in the UofL studies so far.
“I am more of an outlier on the low end, but at 56 years old and nearly 40 years post injury, I think I did great,” he said.
Even Harkema was somewhat surprised that Stifel regained voluntary movement as soon as his early sessions led by Claudia Angeli, assistant professor of bioengineering and director of the epidural stimulation program at KSCIRC.
“I admit we had low expectations of Henry being able to move voluntarily after almost four decades of no movement,” said Harkema, professor of neurological surgery and associate director for KSCIRC. “Even though it supported our theory of the sophistication of the human spinal circuitry, I was stunned when Dr. Angeli was able to find stimulation configurations for him to sit independently and move his toes, ankles, knees and hips in the first sessions. Importantly, this shows that under the right conditions, recovery can happen even decades after injury.”
Now that he has completed his initial part of the study, Stifel is taking part in another study arm in which he will complete another 80 sessions focusing on trunk control and voluntary leg movement.
Once he completes the additional studies, Stifel plans to incorporate training with the stimulator in his daily exercise routine. Although he is not steady enough to stand on his own at home, he will continue that training along with blood pressure regulating, core exercising and any other positive outcomes that might come from this new phase of the study.
“I don’t want to do this study and then shelve it. We accomplished a lot and I want to be able to do more.” Stifel said. “I feel like I won the senior golf tournament, but I still want to beat the kids that have won the Masters. It’s human nature to want more.”
He also is happy to have contributed personally to the overall body of research.
“I think I have helped them move the research needle,” Stifel said. “There have been so many exciting discoveries. Spinal cord injury research has moved from the graveyard of neurological research to interventions that are impacting lives today. This field of research is quickly moving from the traditional fundraising path to one of venture philanthropy and gaining the interest of true capital. Lives are being changed thanks to epidural stimulation, transcutaneous stimulation and the other work being done here and elsewhere.
“This is an amazing research study within the walls of an amazing university. I hope the Louisville community is aware of it and proud of the accomplishments coming from it. It is an amazing time for this field of research.”
Visit Henry Stifel’s blog about his journey with epidural stimulation research at http://henrysjourney.com.
To support spinal cord injury research at the University of Louisville, visit VictoryOverParalysis.org.
UofL medical resident draws on her own experiences to help college students facing illness and disability
When she was growing up, Shannon Strader experienced constant pain and nausea. When she was a senior in high school, she was diagnosed with a rare kidney and vascular disease, Posterior Nutcracker Syndrome, in which the vein from her left kidney is anatomically displaced and compressed between her spine and aorta.
During the summer between high school and college, Strader underwent the first of three surgeries to treat her condition. As a college sophomore, struggling to sustain her college education and social life while navigating her health issues, she looked for ways to connect and share support with other students with similar experiences.
“There was no national organization to support people with all types of disabilities – only specific types of illnesses,” Strader said. Because it is extremely rare, no support group exists specifically for her illness.
So Strader, now a second-year medical resident at UofL, created a blog to share her experience and to connect with other college students with long-term health problems. She went on to establish Bella Soul, a non-profit organization to provide scholarships and emotional support to students facing chronic illness or disability. Strader assembled a board of directors that included college classmates and other advisers, established the 501(c)3 corporation with support from family, friends and her school – the University of Wisconsin – Madison, and began accepting donations.
Bella Soul awarded the first three scholarships in 2013.
“Since then, we have awarded 50 scholarships to young adult students to help with medical bills or other expenses related to their illness or disability,” Strader said. Strader said Bella Soul receives 50-100 scholarship applicants for every scholarship available and has given between 2 and 10 scholarships each year, depending on funds raised that year.
Reviewing all the applicants is time consuming, Strader said, but she is glad to be able to connect with each of the students, who apply by sharing their stories and proof they are students.
“It is exhausting, but all very amazing,” she said.
As an undergraduate, Strader studied neurobiology and stem cell sciences and worked in the regenerative biology lab of James Thomson at the Morgridge Institute for Research at UW – Madison. Her interest in stem cells is motivated by her own illness as well as that of her twin sister, Lauryn, who had cerebral palsy and died when they were 8 years old.
After graduating from UW – Madison, Strader obtained a master’s in biomedical sciences and received her medical degree from Lincoln Memorial University – DeBusk College of Osteopathic Medicine in Knoxville. She chose UofL for her residency training in physical medicine and rehabilitation because of the extensive inpatient opportunities available to the residents at UofL Health – Frazier Rehab Institute. She hopes to pursue clinical care as well as conduct biomedical research into neurological disabilities such as cerebral palsy.
“I came to UofL because the program was one of only a couple of places that offer good inpatient experience caring for individuals with complex disabilities,” she said. “My main goal is to figure out better treatment options for these individuals. Their treatment options have not changed in 20 years.”
UofL scientist receives $6.7 million to learn how metals cause lung cancer
For nearly three decades, John Pierce Wise Sr. has investigated the connection between exposure to metals and cancer, working both in the lab and in the field, reporting significant discoveries about the effects of metals on chromosomes in lung cancer and how those effects differ in humans and in whales.
Wise, professor in the University of Louisville’s Department of Pharmacology and Toxicology, now has received $6.7 million over eight years from the National Institute of Environmental Health Sciences through the Revolutionizing Innovative, Visionary Environmental health Research (RIVER) program to investigate how chromosome instability resulting from exposure to metals leads to lung cancer.
Lung cancer is the leading cause of cancer death in the U.S., and Kentucky has the highest rates of lung cancer incidence and mortality of any state. Despite the widely held perception that lung cancer is simply attributed to smoking, 1 in 5 women and 1 in 12 men who develop lung cancer never smoked. In addition to high rates of cancer, lung cancer has a five-year survival rate of 21%, one of the lowest of any cancer site.
“Lung cancer has a substantial impact on human health, particularly here in Kentucky, and it is time the misconception that smoking is the only cause of lung cancer is dispelled,” said UofL interim president Lori Stewart Gonzalez. “We are grateful for the institute’s confidence in Dr. Wise and our university to lead this work in addressing such a significant health concern. I am excited to see this amazing research continue and expand at UofL thanks to this grant.”
Metals are some of the top environmental causes of human lung cancer, but scientists do not fully understand how the metals cause cancer. Wise’s research has shown that one such metal, hexavalent chromium, causes chromosome instability, in which the chromosomes are increased, deleted or rearranged in inappropriate ways. This chromosome instability can lead to the development of cancer.
Wise has studied metals-induced chromosome instability in humans and animals. Through his field work in sampling skin and blubber from whales, Wise has discovered that while the animals are exposed to hexavalent chromium in the ocean, it results in much less chromosome instability and cancer.
“What’s thought to underlie that is a double-strand break in the DNA helix. In human and whale cells, chromium induces the same number of breaks, so you would expect the same amount of effect on the chromosomes, but you don’t see that,” Wise said. “One of the things we’ve found is that chromium also inhibits the repair of these breaks in humans – you get the breaks and you can’t fix them. In whale cells you get the breaks, but you can fix them. What about whales is protective or corrective? That’s what we’re digging into.”
Wise has assembled a team of researchers from around the world to investigate this process further with the hope that this knowledge ultimately will lead to ways of preventing and reversing metals-induced lung cancer in people.
The research will include laboratory studies and then translate those findings to wildlife and human populations of workers exposed to metals. In addition to Wise, project researchers include KeJian Liu of the University of New Mexico, who will lead lab studies and Tongzhang Zeng of Brown University, who will lead work with human populations. Doctoral students in Wise’s lab and UofL faculty members Sandra Wise, Michael Merchant and Matt Cave also will participate, along with additional researchers in the U.S., Germany, China and Japan.
“UofL is one of the top institutions in the country in research and discovery for how human health is influenced by our environment, and preeminent researchers like Dr. Wise are the reason,” said Kevin Gardner, UofL executive vice president of research and innovation. “This grant is recognition of the incredible contributions Dr. Wise has made to the field and provides ongoing support for continued discovery for years to come.”
RIVER grants are awarded to select investigators who have shown a broad vision and potential for impactful research. They allow the investigator increased flexibility and the freedom to set specific research goals toward a given objective, adjusting the research based on new findings, without seeking new funding. Cave received a RIVER grant in 2017 to conduct research into the effects of environmental exposures on fatty liver disease.
Researchers recommend human clinical trials for CBD to prevent COVID-19 based on promising data
An interdisciplinary team of researchers from several institutions headed by the University of Chicago and including the University of Louisville has found evidence that cannabidiol (CBD), a product of the cannabis plant, can inhibit infection by SARS-CoV-2 in human cells and in mice.
The study, published Jan. 20 in Science Advances, found CBD showed a significant negative association with SARS-CoV-2 positive tests in a national sample of medical records of patients taking the FDA-approved drug for treating epilepsy. The researchers now say that clinical trials should be done to determine whether CBD could eventually be used as a preventative or early treatment for COVID-19.
They caution, however, that the COVID-blocking effects of CBD come only from a high purity, specially formulated dose taken in specific situations. The study’s findings do not suggest that consuming commercially available products with CBD additives that vary in potency and quality can prevent COVID-19.
Scientists have been looking for new therapies for people infected by the coronavirus and emerging variants, especially those who lack access to vaccines, as the pandemic continues across the country and world and as breakthrough infections become more common.
“The Commonwealth of Kentucky has a robust hemp agriculture, so we were pleased to find that pharmaceutical grade CBD is worth testing in future human clinical studies,” said Kenneth Palmer, study coauthor who headed the UofL research team. “In response to the COVID-19 pandemic, our team developed expertise in SARS-CoV-2 infection models and we welcomed the opportunity to collaborate with the University of Chicago team to confirm the efficacy of CBD treatment against SARS-CoV-2.”
Palmer is director of the Center for Predictive Medicine for Biodefense and Emerging Infectious Diseases and the Leona M. and Harry B. Helmsley Charitable Trust Endowed Chair in Plant-based Pharmaceutical Research at UofL. The center houses the Regional Biocontainment Laboratory, one of only 12 regional and two national biocontainment labs in the United States and the only one in Kentucky. Established with support from the NIH to conduct research with infectious agents, the lab includes Biosafety Level 3 facilities built to the most exacting federal safety and security standards.
Researchers from the University of Louisville co-authoring the study with Palmer are Divayasha Saxena, Jon D. Gabbard, Jennifer K. Demarco, William E. Severson and Charles D. Anderson. The research was directed by the University of Chicago and other scientists involved are from the National Argonne Laboratory, the University of Illinois at Chicago and the National COVID Cohort Collaborative Consortium.
CBD: An unexpected avenue for fighting COVID-19
The idea to test CBD as a potential COVID-19 therapeutic was serendipitous. “CBD has anti-inflammatory effects, so we thought that maybe it would stop the second phase of COVID infection involving the immune system, the so-called ‘cytokine storm.’ Surprisingly, it directly inhibited viral replication in lung cells,” said Marsha Rosner, PhD, Charles B. Huggins Professor in the University of Chicago’s Ben May Department of Cancer Research and a senior author of the study.
To see this effect, UofL researchers first treated human lung cells with a non-toxic dose of CBD for two hours before exposing the cells to SARS-CoV-2 and monitoring them for the virus and the viral spike protein. They found that, above a certain threshold concentration, CBD inhibited the virus’ ability to replicate. Further investigation found that CBD had the same effect in two other types of cells and for three variants of SARS-CoV-2 in addition to the original strain.
CBD did not affect the ability of SARS-CoV-2 to enter the cell. Instead, CBD was effective at blocking replication early in the infection cycle and six hours after the virus had already infected the cell.
Like all viruses, SARS-CoV-2 affects the host cell by hijacking its gene expression machinery to produce more copies of itself and its viral proteins. This effect can be observed by tracking virus-induced changes in cellular RNAs. High concentrations of CBD almost completely eradicated the expression of viral RNAs. It was a completely unexpected result.
“We just wanted to know if CBD would affect the immune system,” Rosner said. “No one in their right mind would have ever thought that it blocked viral replication, but that’s what it did.”
The researchers showed that the mechanism by which CBD blocks SARS-CoV-2 replication involves CBD activation of one of the host cell stress responses and generation of interferons, an antiviral cell protein.
Real world data: Patients taking CBD test positive for COVID-19 at lower rates
The researchers wanted scientific data to show that CBD prevents viral replication in live animals. The team showed pretreatment with CBD for one week prior to infection with SARS-CoV-2 suppressed infection both in the lung and the nasal passages of mice. “These results provide major support for a clinical trial of CBD in humans,” said Rosner.
And the success of CBD wasn’t limited to the laboratory: An analysis of 1,212 patients from the National COVID Cohort Collaborative revealed that patients taking a medically prescribed oral solution of CBD for the treatment of epilepsy tested positive for COVID-19 at significantly lower rates than a sample of matched patients from similar demographic backgrounds who were not taking CBD.
The potential for CBD to treat patients recently exposed to or infected by SARS-CoV-2 does not precede the first lines of defense against COVID-19, which are to get vaccinated and follow existing public health guidelines for masking in indoor spaces and social distancing. But the published results offer a potential new therapeutic, something still needed as the pandemic rages on.
“A clinical trial is necessary to determine whether CBD is really effective at preventing or suppressing SARS-CoV-2 infection, but we think this may have potential as a prophylactic treatment,” said Rosner. “Maybe you’re in a hot spot or you think you might have been exposed or you’ve just tested positive — that’s where we think CBD might have an effect.”
Not your dispensary’s CBD
The research team emphasized that the COVID-blocking effects of CBD were confined strictly to high purity, high concentrations of CBD. Closely related cannabinoids such as CBDA, CBDV and THC, the psychoactive element enriched in marijuana plants, did not have the same power. In fact, combining CBD with equal amounts of THC actually reduced the efficacy of CBD.
“Going to your corner bakery and buying some CBD muffins or gummy bears probably won’t do anything,” said Rosner. “The commercially available CBD powder we looked at, which was off the shelf and something you could order online, was sometimes surprisingly of high purity but also of inconsistent quality. It is also hard to get into an oral solution that can be absorbed without the special, FDA-approved formulation,” Rosner said.
Furthermore, CBD use is not without potential risks. It appears to be extremely safe when consumed in food or drink, but methods of use such as vaping can have negative side effects, including potential damage to the heart and lungs. It’s also not well studied in certain populations, such as pregnant people, and so should be used only under the supervision of a physician and with caution.
While the study’s results are exciting, additional study is needed to determine the precise dosing of CBD that is effective at preventing SARS-CoV-2 infection in humans as well as its safety profile and any potential side effects.
“We are very eager to see some clinical trials on this subject get off the ground,” Rosner said. “Especially as we are seeing that the pandemic is still nowhere near the end — determining whether this generally safe, well-tolerated, and non-psychoactive cannabinoid might have anti-viral effects against COVID-19 is of critical importance.”
Rosner was also pleased that this research project was a case study in the power of scientific collaboration by bringing together a highly interdisciplinary group of researchers. Senior authors listed on the paper came from three different research universities and from departments as diverse as microbiology, molecular engineering, cancer biology and chemistry.
“This was truly a team-science effort, and that’s something that really excites me,” said Rosner. “From clinicians to David Meltzer’s group who did the patient analysis to virologists like Glenn Randall, and it goes on and on. This is the way science should be carried out.”
UofL researchers develop gene therapy to regenerate heart cells
Study authors in the UofL Institute of Molecular Cardiology, (l. to r.) Qinghui Ou, Xian-Liang Tang, Tamer Mohamed, AbouBakr Salama and Riham Abouleisa
UofL physiatrists provide key role in RETAIN Kentucky, a service to help people return to work after injury or illness
University of Louisville physical medicine and rehabilitation physicians Matthew Adamkin and Priya Chandan are helping lead a new initiative in Kentucky, funded by the U.S. Department of Labor, to help people with illnesses or injuries keep working and avoid long-term disability.
The program, RETAIN Kentucky, which stands for Retaining Employment and Talent after Injury/Illness Network, is a free service for Kentucky residents who have experienced an illness or injury outside the workplace to help them obtain services or accommodations so they can continue working.
“The benefits of maintaining or going back to work are immense beyond the financial – psychosocial, physical, mental – so it’s much better than ending up on long-term disability,” Adamkin said. “We have had stroke patients who otherwise would have gone on disability who now are returning to work. We have folks who have had COVID who were hospitalized or had prolonged illness who are working on getting back to work.”
Once an individual is enrolled in RETAIN, a return-to-work coordinator helps them access existing resources, such as workplace accommodations or assistance with transportation, rent or utilities. The coordinator will help the individual develop a return-to-work plan that provides personalized support including assistance with health care and employer communications.
In the pilot phase of the program, Adamkin and Chandan, faculty members with the UofL School of Medicine, advised program leaders and were responsible for more than 60% of referrals to the program through UofL Health – Frazier Rehab Institute. Now, Kentucky is one of only five states to receive funding from the U.S. Department of Labor to expand the program in its second phase.
“At Frazier we see such a wide variety of patients – stroke, spinal cord injury, COVID patients – but regardless of their diagnosis, whether they rolled their ankle playing flag football over the weekend or had a stroke, everybody benefits because there are so many resources available,” Adamkin said.
RETAIN Kentucky is led by Kentucky’s Department of Workforce Investment in the Education and Workforce Development Cabinet. Implementation is overseen by the University of Kentucky, with a subaward to UofL and Frazier Rehab Institute. UK Healthcare and UofL Health are the leading health organizations for the project, which aims to enroll 3,200 people over four years from across the state. Adamkin and Chandan also are working to educate faculty, residents and medical students in the UofL School of Medicine about the program and the benefits of these services on patients’ quality of life and conducting research to determine how the program performs in terms of both health and employment outcomes.
If you or someone you know has experienced an injury or illness outside the workplace and would benefit from assistance in returning to work, visit https://www.kyretain.org or call 859-562-3251.
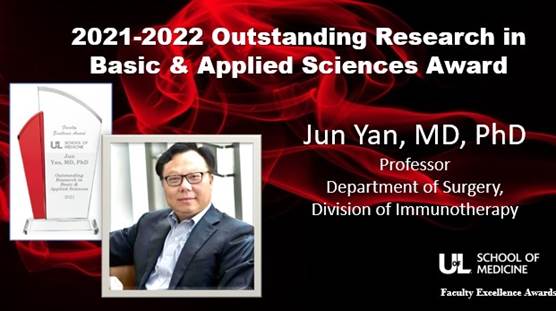
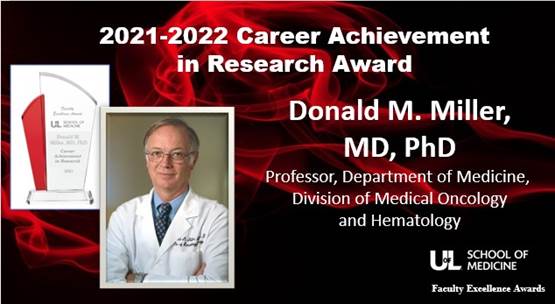
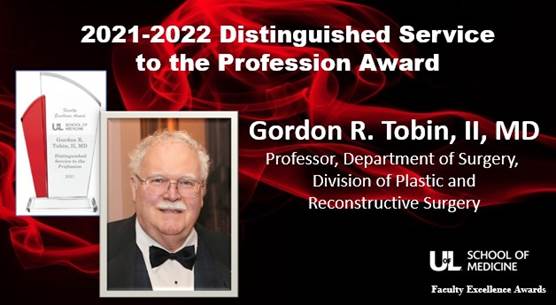
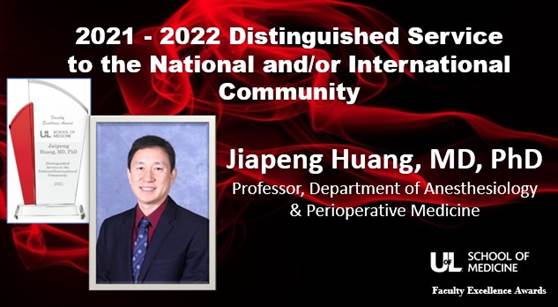
ULSOM 3rd Annual Faculty Excellence Awards
The University of Louisville School of Medicine held its 3rd annual Celebration of Faculty Excellence on Tuesday, November 30. More than 80 people were in attendance and more joined virtually to learn of the 2021 award winners. The ULSOM Faculty Excellence honors those who bring distinction to our institution through Outstanding Scholarship, Research and Creative Activity Awards, Distinguished Service Awards, and Educator Awards.



School of Medicine appoints Assistant Dean for Faculty Affairs & Advancement
Christopher Seals, Ph.D., has been selected by the University of Louisville School of Medicine as the new Assistant Dean for Faculty Affairs & Advancement. In addition, Seals has been appointed as Assistant Professor in the School of Medicine Dean’s Office.
“We are excited for Dr. Seals to be joining our team. His professional experience brings a history and passion for diversity, equity and inclusion work. He is a distinguished collaborator and communicator that will provide our faculty, residents and fellows with a culture that empowers all,” said Toni Ganzel M.D., M.B.A., dean of the School of Medicine.
In this position, Seals will function as an advocate for under-represented faculty in the School of Medicine. He will work collaboratively with the Vice Dean of Faculty Affairs and Advancement to support and expand initiatives with faculty diversity, inclusion and recruitment, and retention. He will also collaborate with the Vice Dean for Graduate Medical Education and the Assistant Dean for CME and Professional Development to provide a strong infrastructure of innovative resident and fellow programs and services that promote resident and fellow retention as faculty members, as well as work with the Chief Diversity Officer for the School of Medicine and other Offices of Diversity and Inclusion at the Health Sciences Center and the main campus of University of Louisville.
“The Assistant Dean position will allow me to apply my knowledge in an administrative role that will directly impact faculty and their ability to serve the medical community and advance their own careers. As a Kentucky native, I am excited for the opportunity to return to my alma mater and use my considerable experience in diversity and inclusion, collaborating, and professional development to assist the SOM in meeting its goals,” Seals said of accepting his new role.
Seals has twelve years of leadership in higher education, most recently at the University of Illinois where he served as the Coordinator of Curriculum and Assessment for the College of Veterinary Medicine and a Tenure Track Assistant Professor of Education in the Veterinary Clinical Medicine (VCM) department. He received his PhD in Education Psychology & Educational Technology from Michigan State University in 2018. He completed his Master of Education in Education & Counseling Psychology and Personnel Services in 2011 and a Bachelor of Arts in 2008 from the University of Louisville.
Seals will begin his new role March 1, 2022.
The black death still has lessons to share
A live microscopy image of macrophages, white blood cells that mediate innate immunity, infected with Yersinia pestis, shown in red. UofL photo by Matthew Lawrenz and Tiva VanCleave, a former doctoral student in Lawrenz’s lab.
Bubonic plague may not seem like a significant problem in the world today. While it killed millions of people in Europe in the Middle Ages and was known as the “black death,” it mostly has faded from public concern.
Microbiologists at the University of Louisville study Yersinia pestis, the bacteria that causes bubonic plague, however, because it has the potential to be used as a bioweapon and it provides knowledge that may apply to efforts to defeat other bacteria. Through this work, they have made an important discovery about a molecule secreted by Y. pestis and other bacteria that helps defeat the host’s immune defenses, allowing the bacteria to infect its hosts.
Sarah Price, a doctoral student researcher, and her mentor, Matthew Lawrenz, associate professor of microbiology and immunology, have found that yersiniabactin, a small molecule secreted by Y. pestis, gathers zinc, a necessary element for bacterial replication. This discovery may have implications in other infections as well since bacteria causing pneumonia, sepsis and other illnesses also are known to release yersiniabactin.
“While yersiniabactin’s role in iron acquisition has been well known for over 30 years, we were surprised to see its significant impact on zinc acquisition during Y. pestis infection,” Price said “This is very exciting because it helps us understand how Y. pestis and other bacteria acquire nutrients that allow them to cause disease.”
Invading bacteria as well as the hosts they infect all require iron, zinc and other metals in order to grow. The host’s immune system employs a strategy called nutritional immunity to protect against these bacterial infections, sealing the metals away from the bacteria.
It has been known for many years that yersiniabactin defeats this defense by stealing away iron and delivering it into the bacterial cells. Price and Lawrenz have discovered that the molecule also is involved in securing zinc and perhaps even other metals to assist Y. pestis infection.
Yersiniabactin also is used by Escherichia coli, which causes a multitude of infections such as intestinal illness and kidney infections, and Klebsiella pneumoniae, which causes pneumonia and sepsis. These more common diseases can be life-threatening and multidrug-resistant infections. The new understanding may lead to additional strategies for controlling infection by all of these bacteria.
An article describing the research published Oct. 29 in PNAS provides details about how the researchers determined that yersiniabactin was responsible for the collection of not only iron, but zinc. Price is first author on the publication, “Yersiniabactin Contributes to Overcoming Zinc Restriction during Yersiniapestis Infection of Mammalian and Insect Hosts.” Lawrenz, associate professor of microbiology and immunology, is senior author, and researchers from the University of Kentucky, Washington State University and the University of Illinois also contributed to these studies.
“With this understanding of the broader role of yersiniabactin in plague infection, we can explore further to understand its role in enabling other bacteria to infect a human or other host,” Lawrenz said. “If this mechanism holds true across these bacteria, it may be possible to develop a drug or vaccine that could inhibit yersiniabactin’s effectiveness, thus preventing all of these infections.”
Bubonic plague most often is transmitted to humans through the bite of an infected flea, usually carried by a rodent. By not handling animal carcasses, preventing flea bites and avoiding contact with bodily fluids of those infected, the spread of bubonic plague is largely controlled. However, since human-to-human transmission is possible, mortality from an infection ranges from 30-90% and no vaccine is available to prevent the infection, it remains an important pathogen for research. In addition, Y. pestis, has the potential for weaponization and is considered a bioterrorism threat.
Lawrenz, Price and their colleagues conduct research within the UofL Center for Predictive Medicine for Biodefense and Emerging Infectious Diseases, which focuses on the development of prevention and treatment strategies for infectious diseases and other harmful pathogens. Its researchers utilize the UofL Regional Biocontainment Laboratory, a member of the National Institute of Allergy and Infectious Diseases network of 12 regional and 2 national biocontainment laboratories for studying infectious agents. The lab includes Biosafety Level 3 facilities built to the most exacting federal safety and security standards to protect researchers and the public from exposure to the pathogens being investigated.
The center’s researchers were called upon in early 2020 to develop tests and prevention and treatment strategies against SARS-CoV-2, the virus that causes COVID-19. This work continues.
Kosair Charities grants $6.4 million to UofL for children’s health programs
Luke Madson on a specially designed pediatric treadmill for therapy at the Kosair Charities Center for Pediatric Neurorecovery
The Kosair Charities Center for Pediatric NeuroRecovery at the University of Louisville brings about recovery for children with spinal cord injuries through therapies developed by the center’s director, Andrea Behrman, professor in the UofL Department of Neurological Surgery, and her team within the Kentucky Spinal Cord Injury Research Center.
Kosair Charities, which supported the program at its inception in 2014, has extended that support through 2026 with a new grant for $5.5 million over five years.
Children in the clinical and research programs of the Center for Pediatric NeuroRecovery are treated with innovative, science-based therapies such as activity-based locomotor training, neuromuscular electrical stimulation and transcutaneous spinal stimulation. These therapies have led to improved strength, abilities and overall health for the children in ways their families thought would not be possible.
“We went from feeling hopeless to hopeful after just one conversation with Dr. Behrman,” said Kylee Hoelscher who, with her husband and older daughter, moved from California to Louisville in 2016 so their then-six-year-old daughter Eden could continue therapy.
“This is the only program in the world that offers hope for children with a spinal cord injury,” Hoelscher said. “When she started, Eden could not even sit up on her own and attended school at home. Now she goes to school independently and has sleepovers with friends. She rock climbs. She plays tennis. What they’re doing for her is life-changing.”
“We are grateful to Kosair Charities for their continued support for the Center for Pediatric NeuroRecovery, a remarkable program that gives hope for recovery to children with spinal cord injuries – hope and care they can find almost nowhere else,” said UofL President Neeli Bendapdudi. “This support, along with that of other pediatric research and clinical care programs at UofL, will help us fulfill our commitment to advancing our health, not only for children in Louisville and Kentucky, but the world over.”
In addition to the multi-year $5.5 million in new funding for pediatric neurorecovery, Kosair Charities has designated $900,000 this year for other pediatric programs at UofL:
- $475,000 for the Kosair Charities Division of Pediatric Forensic Medicine, led by Melissa Currie, professor of pediatrics, to support education, research and advocacy to help curb all forms of child maltreatment.
- $225,000 to purchase cardiorespiratory monitors at the UofL Health – UofL Hospital Neonatal Intensive Care Unit, led by Tonya Robinson. These cardiorespiratory monitors provide real-time and trended vital signs, allowing for a comprehensive evaluation of an infant’s current status and of changes occurring before a devastating event. The monitors assist in determining the causes of medical events and help prevent them from happening again.
- $200,000 for pediatric cancer immunotherapy research at UofL Health – Brown Cancer Center, directed by Jason Chesney, that will allow the center to build on the cancer immunotherapy drug discovery work begun in 2020 that already has revealed new small-molecule inhibitors.
“Everything we do is for children, whether it be with spinal cord injuries, cancer, those born prematurely, or vulnerable – every child who has specialized needs – they are the motivation behind everything we do,” said Keith Inman, president of Kosair Charities. “There’s no better investment than the children in our community, and we simply cannot do this work without partners like the University of Louisville. The partnership of UofL and Kosair Charities helps ensure so many children have the healthiest lives possible.”
At the Center for Pediatric NeuroRecovery, the funding from Kosair Charities will support further advances in therapy for children with spinal cord injury, as well as research and training for future researchers and providers. It also will enable the program to accept younger and medically complex children, develop a teen-focused recovery-based program and study neuromodulation, a way to stimulate the spinal cord and improve mobility and health.
“Children with spinal cord injury are at risk for multiple medical and health complications. This grant from Kosair will allow us to expand our focus to improve areas of their health beyond movement,” Behrman said. “This will not only get these children physically better but help them have a healthy life.”
The Madson family also relocated to Louisville for this program, moving from the Minneapolis area to ensure their son Luke could continue the therapy, based at UofL Health – Frazier Rehab Institute.
“The more Luke moves, the more alive he is,” Sarah Madson said of her now-two-year-old son, who was the youngest child to start the program at 15 months. “When we arrived, he was crawling on the ground, maybe doing little circles, with no forward movement. He is now walking in a walker everywhere and engaging with the world. This program has meant everything to us.”
The grant announced today brings Kosair Charities’ total support for the center to $13 million.
In April, UofL and Kosair Charities celebrated a milestone of topping $50 million in gifts from Kosair Charities to UofL since 1982. The grants announced today bring that total to $56.8 million.
First-in-world heart implant: Woman receives novel type of artificial heart at UofL Health – Jewish Hospital by University of Louisville physicians
Cardiothoracic surgeons with UofL Health – Jewish Hospital and the University of Louisville performed the world’s first Aeson® bioprosthetic total artificial heart implantation in a female patient on Sept. 14, 2021. Photo by UofL Health.
A cardiothoracic surgical team with UofL Health – Jewish Hospital and the University of Louisville has performed the world’s first Aeson® bioprosthetic total artificial heart implantation in a female patient. The investigational device, currently intended as a bridge to heart transplant, is part of an Early Feasibility Study (EFS) sponsored by CARMAT, a French medical device company, in partnership with UofL, UofL Health – Jewish Hospital and the UofL Health – Trager Transplant Center.
Led by cardiothoracic surgeons Mark Slaughter, M.D., and Siddharth Pahwa, M.D., both of UofL Health - UofL Physicians and the UofL School of Medicine, the team performed the implant of the device on Sept. 14, 2021 at UofL Health – Jewish Hospital. The same team completed the nation’s second implantation in a male patient last month, also at Jewish Hospital.
“For the other half of the world’s population, completion of this procedure by the Jewish Hospital team brings new hope for extended life,” said Slaughter, UofL Health surgical director of heart transplant and professor and chair of the Department of Cardiovascular and Thoracic Surgery in the UofL School of Medicine. “Size limitations can make it harder to implant artificial hearts in women, but the Aeson artificial heart is compact enough to fit inside the smaller chest cavities more frequently found in women, which gives hope to a wider variety of men and women waiting for a heart transplant and increases the chances for success.”
More than 3,500 individuals are awaiting a heart transplant in the U.S. and 900 of them are women. There are few treatment options for patients with biventricular heart disease, meaning both the left and right sides of the heart are not pumping blood adequately. The Aeson device is designed to solve the limitations of current left-ventricular assist devices (LVAD), which pump blood in just one chamber, by pumping blood in both heart chambers. Aeson also contains pressure sensors that estimate the patient’s blood pressure and automatically adapts cardiac output according to the sensor information. It is fully implanted as a heart replacement and powered by a portable external power supply.
During this procedure, the Aeson total artificial heart was implanted into a 57-year-old Kentucky woman with severe biventricular heart failure during an eight-hour surgery. The recipient, whose identity is being withheld upon request, was referred to the Advanced Heart Failure Therapies Program at Jewish Hospital earlier this year with end-stage heart failure and had undergone cardiac surgery years before. The patient is recovering well in the cardiovascular intensive care unit (CVICU). Jewish Hospital is just one of four programs in the nation approved to perform this clinical trial procedure.
“The varying pumping ability of the Aeson device increases its viability among more patients,” said Pahwa, UofL Physicians cardiothoracic surgeon and assistant professor in the UofL Department of Cardiovascular and Thoracic Surgery. “While other devices are set at a fixed rate or create a continuous flow, CARMAT has developed the Aeson to automatically adjust the flow, creating an improved performance to meet the body’s changing blood flow needs.”
Currently, the Aeson artificial heart is tested as a bridge to transplant for patients with end-stage biventricular heart failure, allowing more time for the patient to receive a permanent heart organ transplant. The device already has been approved for such use in Europe, where approximately 20 devices have been implanted. It currently is being tested in the U.S. as part of a feasibility study approved by the Food and Drug Administration. The first Aeson artificial heart in North America was implanted in a male patient in July at Duke University Medical Center. The second implantation, also in a male patient, was performed at Jewish Hospital in August. This third North American implantation is the first to involve a female patient.
“Even as we have fought this deadly pandemic, our researchers and health care providers have also been on the front lines of improving care and quality of life for not only Kentuckians, but for people around the world,” said Kentucky Gov. Andy Beshear. “I am proud that UofL, Jewish Hospital and their doctors are leading the world in implanting this promising and innovative device that could offer hope and time to thousands of people, including our wives, mothers and other loved ones, in coming years.”
Stéphane Piat, chief executive officer of CARMAT, said, “This third implant in the U.S. was a landmark event not only because it allowed us to finalize the enrollment of the first cohort of patients of the EFS, but very importantly because it is the first time ever that our device has helped a woman suffering from heart failure. This achievement confirms that the size limitations for adults are minimal, which makes us very confident in Aeson’s potential to become a therapy of choice for a broad patient population.”
Preclinical research for CARMAT’s artificial heart began at UofL more than five years ago. Researchers at UofL’s Cardiovascular Innovation Institute (CII) tested Aeson’s autoregulation capability, which allows the device to adapt its flows according to the patient’s needs by detecting changes of pressure in the device. UofL researchers have conducted preclinical testing of artificial heart components and mechanical assist devices at CII for many years, testing some portion of nearly every mechanical assist device that is commercially available today.
Jewish Hospital and the University of Louisville share a storied history in advancing heart care. Highlights include:
- Aug. 24, 1984: Kentucky’s first heart transplant performed at Jewish Hospital by UofL physicians
- July 2, 2001: The world’s first AbioCor® artificial heart was implanted at Jewish Hospital by UofL physicians, led by cardiothoracic surgeon Laman Gray, M.D.
- Dec. 21, 2011: Kentucky’s first transcatheter aortic-valve replacement (TAVR) performed at Jewish Hospital by UofL physicians
- Jan. 18, 2015: Kentucky’s first HeartMate 3TM left ventricular assist device (LVAD) implanted at Jewish Hospital by UofL physicians
- Feb. 21, 2018: UofL Health - Trager Transplant Center’s 500th heart transplant performed at Jewish Hospital
- June 14, 2019: The first EvaHeart®2 LVAD implanted as bridge to transplant at UofL Health - Trager Transplant Center
- April 22, 2021: UofL Health - Trager Transplant Center’s 1000th TAVR performed at Jewish Hospital
“This world-first artificial heart implant into a female patient is another demonstration of UofL Health’s commitment to provide both the world-class care of today and develop the world-class standards of tomorrow,” said John Walsh, chief administrative officer of Jewish Hospital. “We celebrate this first as a milestone and recognize the hard work of Drs. Slaughter and Pahwa and the entire team. The true impact of their work will be measured in the dozens, hundreds and thousands of lives improved in the years to come.”
The patient who received the nation’s second Aeson implant, on Aug. 20, 2021, continues to improve at Jewish Hospital. An update is expected in the coming weeks.
UofL Health – Frazier Rehab Institute to celebrate new location for unique Louisville accessible fitness gym
UofL Health and Louisville leaders are celebrating the new home of UofL Health – Frazier Rehab Institute's Community Fitness and Wellness gym, now located on the ground floor of Medical Plaza II, 250 E. Liberty Street. The UofL Health – Frazier Rehab Institute team provides rehabilitation services through a wide-variety of inpatient and outpatient programs for adults and children with disabling conditions including, but not limited to brain injury, spinal cord injury, stroke, and movement disorders.
“Quality care for those living with physical impairments is now even more accessible,” said Tom Miller, CEO of UofL Health. “Our mission is to build a stronger community by improving the health and quality of life for everyone we serve. This is yet another example of our commitment to do just that.”
The CFW is a fully wheelchair-accessible community gym with state-of-the-art equipment and professional staff trained to provide specialized activity-based exercise interventions for people with disabilities. Individualized exercise plans are developed to meet each client’s personal fitness goals.
“Over the past seven decades, Frazier Rehab has become a recognized leader in rehab care both regionally and nationally,” said Cathy Spalding, Chief Administration Officer of Frazier Rehab Institute. “Frazier Rehab has helped thousands of people regain both mental and physical strength that they thought would be nearly impossible to get back after their illness or injury.”
In 2006, Elizabeth Fust suffered a spinal cord stroke that left her paralyzed. She has been a member of the CFW gym since it first opened back in 2007. Fust is also currently serving on the UofL Health - Frazier Rehabilitation Institute Board of Trustees and is the founder of the 501(c)(3) charity, Gathering Strength, Inc., in Louisville.
“The CFW gym has been vital to maintaining and improving my health because it is the only place in Louisville that has wheelchair accessible exercise equipment and specially trained staff who are not afraid to work with people like me, who have disabling conditions,” Fust said. “It is unique also because it offers an opportunity for me to be around many people who have similar injuries and challenges, and we can support each other.”
This year the CFW moved to the ground floor of Medical Plaza II from Frazier Rehab’s 9th floor gym, located at 220 Abraham Flexner Way. The new location is not only more accessible, but also offers opportunities to grow and expand services. Thanks, in part, to a $190,000 dollar grant from the Craig H. Neilsen Foundation the CFW is upgrading equipment, further marketing the program, and growing its membership through a partnership with Gathering Strength, Inc.
“Through our Creating Opportunity & Independence (CO&I) portfolio, the Craig H. Neilsen Foundation is proud to support UofL Health – Frazier Rehab Institute’s Community Fitness and Wellness gym and the vital opportunities it provides to enhance the health and wellbeing of people living with spinal cord injury,” said Darrell Musick, CO&I Program Officer.
To learn more about UofL Health – Frazier Rehab Institute's Community Fitness and Wellness gym, visit UofLHealth.org or call them at 502-582-7411.
Neal Dunlap tapped to lead Department of Radiation Oncology
Neal Dunlap, M.D., on October 1 will become the new Chair of the University of Louisville Department of Radiation Oncology.
Dr. Dunlap served as Vice Chair and Professor of the Department of Radiation Oncology before accepting his new role. In addition, he serves as the Residency Program Director for the department since 2017 and Associate Director of the Head & Neck Multidisciplinary Clinic. Previously, he held an academic endowed chair appointment through Humana Professorship in Clinical Trials Research at the UofL Brown Cancer Center.
"The Department of Radiation Oncology consists of a group of dynamic faculty and staff who are committed to the advancement of cancer care in Louisville and the Commonwealth. I am excited by the prospect of deepening our relationship with this community to expand access to advanced cancer care and clinical trials, train the next generation of physicians, and promote patient health and dignity," Dunlap said of accepting his new role.
Dr. Dunlap earned his medical degree from the University of Cincinnati College of Medicine. He completed his internship at University of Cincinnati’s University Hospital, and his residency at the University of Virginia Medical Center in Charlottesville. His clinical focus is primarily on multidisciplinary approaches to the treatment of lung cancer, esophageal cancer, head & neck cancers, and liver cancers. His research interests include the application of new treatment technologies in treatment of lung, liver, and head & neck malignancies to improve outcomes and reduce side effects. He currently has investigator-initiated trials open for the re-treatment of lung cancers after previous radiation and the evaluation of early radiation-induced lung injury with 4-dimensional CT. He is currently the institutional principal investigator for multiple national cooperative group studies through NRG/RTOG in the treatment of lung and head & neck cancers. He is member of the American Society for Radiation Oncology.
“I am confident that Dr. Dunlap has the leadership skills, experience and expertise to build on current strengths of the department and to also move it forward in innovative ways,” said Toni Ganzel, M.D., M.B.A., dean of the School of Medicine.
Long-time UofL staff and faculty member joins School of Medicine as Chief of Staff
The University of Louisville School of Medicine has named Glenn Gittings, PhD., as its new Chief of Staff.
In this position, Gittings will provide support with planning, monitoring and implementing the strategic agenda for the school, serving in the capacity of advisor to Dean Toni Ganzel in interactions with colleagues across the schools and institution to ensure institutional alignment with strategic initiatives. He will collaborate with senior leaders and executives, external affiliate leadership, and other external partners on projects that support the missions and strategic priorities, including enterprise alignment, strategic planning, security and other compliance initiatives. Gittings will also lead the School of Medicine Advancement, Retention and Training (SMART) Staff Development Program designed to engage staff in professional and personal development efforts through a number of new initiatives such as mentoring, professional development, community outreach and engagement, recognition and reward, wellness, and a staff retreat.
“I am thrilled to welcome Dr. Gittings to our administrative team. He brings a great deal of experience in the areas of strategic planning, staff development and stakeholder relations, which will provide tremendous support to the School of Medicine priorities of supporting our faculty, residents, staff and students,” said Toni Ganzel, M.D., M.B.A., dean of the School of Medicine.
A long-time staffer and faculty member, Gittings has spent the last 19 years in progressive higher education and the nonprofit sector with experiences at multiple institutions and organizations. He previously served as the Director of the Student Activities Center & Special Programs on the Belknap campus at the University of Louisville where he fulfilled the role of student union management, First Year Initiative programming, Parent & Family Relations, and External Relations for the division of Student Affairs. Gittings has previous higher education experience in Advancement/Development, Alumni Relations, Assessment, Diversity & Inclusion, Educational Nonprofits, Enrollment Management, External Relations, Event Planning, HR, International Service Learning Program Faculty (Philippines, Trinidad & Tobago), Parent & Family Relations, SACS Accreditation, Sponsorships, Staff Senate, Strategic Planning, Student Union Mgmt., VPSA Special Projects, and Welcome Week/First Year Experience. He also served as a UofL Staff Senator including a role on the Staff Senate Executive Committee.
Gittings is very active in regional and national professional organizations through research opportunities, publications, committee membership, conference presentation, and conference attendance. He served nationally as chair of the NASPA Student Affairs Fundraising and External Relations Knowledge Committee, publishing books, articles, online short courses, and conference presentations on the topic of higher education fundraising. For more than 10 years, he has been a long-standing graduate Adjunct Faculty member for UofL’s College of Education in both the Higher Education Administration program and the College Student Personnel program.
Gittings earned both his bachelor’s degree and Ph.D. from University of Louisville and master’s degree from Western Kentucky University and his dissertation research highlighted key student and institutional factors affecting doctoral student persistence. He and his spouse, Jennifer, have two daughters ages 10 and 7.
Gittings began his new role August 2.
UofL researchers find more health benefits of living in a greener environment
Trees are planted in South Louisville for the UofL Green Heart Project, an ongoing assessment of the effects of neighborhood greenness on individual health.
Evidence is growing that living in areas of high greenness, surrounded by trees, shrubs and other vegetation, has beneficial effects on human health. Researchers at the University of Louisville’s Christina Lee Brown Envirome Institute and other colleagues recently published two studies showing positive effects of greenness: one on cancer survival and the other on depressive symptoms.
In the first study, UofL researchers Aruni Bhatnagar, professor of medicine and director of the Envirome Institute, Ray Yeager and Daniel Riggs, with Carver Coleman and Arden Pope of Brigham Young University and others, analyzed retrospective data from more than 5.5 million cancer patients and survivors from 2003 to 2016. They found that cancer patients in greener counties lived longer than those in counties with less greenness. The protective effects of greenness against cancer mortality were seen with both males and females and individuals of all ages, but were more pronounced at urban locations. Individuals with cancers that were highly survivable – such as breast, prostate and skin cancer – benefitted more from greenness than those with cancers with low survival rates such as brain, esophageal, liver, lung and pancreatic cancer.
The study, “Greenness, air pollution, and mortality risk: A U.S. cohort study of cancer patients and survivors,” published in the journal Environment International, evaluated associations between greenness and fine particulate matter in the air on causes of death in a large group of cancer patients and survivors in the United States.
“This is the largest study of the relationship between greenness and cancer mortality, and it provides clear evidence that living in green areas is beneficial to cancer patients,” said Bhatnagar “However, we do not yet understand why greenness protects against cancer mortality. Much more remains to be done to see whether greenness benefits cancer patients by lowering mental stress and anxiety or by reducing the levels of air pollutants or whether some other mechanisms are at play.”
The study also found that cardiopulmonary disease, but not cancer, was associated with higher levels of fine particulate air pollution. Mortality from cardiopulmonary causes – stroke, heart attack or COPD – was not affected by county greenness, except in rural locations.
Greenness and depression
A second study, led by Kandi Walker and Joy Hart, professors in the UofL Department of Communication, Bhatnagar and other researchers in the Envirome Institute, found that people’s satisfaction with levels of greenness in their neighborhood was associated with lower levels of self-reported depressive symptoms.
The researchers surveyed participants about their perceptions of greenness in their neighborhoods and their mental health symptoms and found that those who were more satisfied with the greenness surrounding their homes also reported lower depression symptoms on a health survey, the Patient Health Questionnaire-9.
The 44.5% of survey participants who reported they were satisfied with the level of greenness in their neighborhood collectively scored better on the health questionnaire for depression.
“Given the pervasiveness of depression in the U.S. population, any changes that can reduce depression are essential, particularly those that can affect a large number of people,” Hart said. “The findings of this study suggest that greening interventions that focus on greenness satisfaction may be a strategy to reduce depression in urban populations.”
The study, “The importance of urban planning: Views of greenness and open space is reversely associated with self-reported views and depressive symptoms,” was published in July in the journal Population Medicine.
South Louisville study participants needed
Participants in the greening satisfaction study were part of the Health, Environment and Action in Louisville (HEAL) study of the Great Heart Project, which is an ongoing assessment of the effects of neighborhood greenness on individual health. Additional participants are needed for the HEAL Study by the end of September. More information is available on the HEAL Study website.
“Together, these studies add weight to the importance of trees, shrubs and other vegetation in urban areas in benefitting and nurturing human health. Accumulation of such evidence strengthens the case that increasing greenness in urban locations can decrease the high rates of non-communicable diseases in cities,” Bhatnagar said. “And since greenness improves health in general, it may also be effective against infectious disease.”
University of Louisville cardiac surgery team second in U.S. to implant new artificial heart
A University of Louisville cardiac surgery team at UofL Health - Jewish Hospital is the second in the United States to implant a new experimental advanced total artificial heart within the framework of an early feasibility study.
The team, led by Mark Slaughter, M.D., professor and chair of the Department of Cardiovascular and Thoracic Surgery in the UofL School of Medicine and lead cardiothoracic surgeon at UofL Health – Jewish Hospital, performed the implant of the investigational device on Aug. 20.
The artificial heart, Aeson®, developed by French medical device company CARMAT, serves as a bridge to transplant for patients with end-stage biventricular heart failure – heart disease affecting both left and right sides of the heart – allowing more time for the patient to receive a permanent heart organ transplant. More than 3,400 individuals in the U.S. currently are awaiting a heart transplant and there are few other treatment options for patients with biventricular heart disease.
“We are excited to bring this new technology to patients in Kentucky and the surrounding region and be one of the first U.S. centers to implant this new total artificial heart,” Slaughter said. “This device has the potential to save the lives of critically ill patients suffering from biventricular heart failure who currently have very limited treatment options.”
The new total artificial heart was implanted into a middle-aged man from Southern Indiana with severe biventricular heart failure during a seven-and-a-half-hour surgery. The recipient, whose identity is being withheld upon request, was referred to the advanced heart failure program at Jewish Hospital. The patient currently is doing well in the cardiac surgery ICU.
The new device is designed to solve limitations of left-ventricular assist devices (LVAD), which pump blood in just one chamber, by pumping blood in both heart chambers. Aeson also contains biosensors that detect the patient’s blood pressure and position and automatically adapts cardiac output according to the sensor information. It is fully implanted as a heart replacement and powered by a portable external power supply.
“We are honored that our device is implanted at UofL Health - Jewish Hospital, which is recognized throughout the United States for its quality of care and cardiovascular research” said Stéphane Piat, chief executive officer of CARMAT. “I would like to congratulate the teams at the Jewish Hospital, the University of Louisville, as well as our technical and medical staff, on this exceptional milestone for both patients and our company.”
The device is medically approved in Europe, where approximately 20 have been implanted. The first Aeson artificial heart in North America was implanted in July at Duke University.
This is not the first time University of Louisville physicians and Jewish Hospital have made artificial heart history. Just over 20 years ago, on July 2, 2001, UofL cardiothoracic surgeon Laman Gray led the surgical team that implanted the first self-contained artificial heart in the United States at Jewish Hospital. The AbioCor artificial heart was implanted into Robert Tools, who lived five months on the device. The UofL surgical team also performed the first heart transplant in Kentucky at Jewish Hospital in 1984.
Renowned cardiac imaging and atherosclerosis prevention researcher joins UofL School of Medicine as chief of cardiology
Dinesh Kalra, M.D., will join the faculty of the University of Louisville Department of Medicine as chief of the Division of Cardiovascular Medicine on Sept. 1. He also will serve as professor of medicine and Endowed Chair of Cardiovascular Innovations.
Kalra comes to UofL from Rush University Medical Center in Chicago, where he was director of advanced cardiac imaging, director of the infiltrative cardiac disease program and director of the lipid clinic. He is internationally renowned for his work in advancing the understanding of cardiac computerized tomography (CT) and magnetic resonance imaging (MRI), and lipidology, especially as it relates to finding new ways to prevent atherosclerosis.
“I am proud to be part of an exceptional institution like UofL with a rich history and tradition of excellence, innovation and research,” Kalra said of his new role at UofL. “The program has a very strong reputation for clinical training and outstanding patient care. The resident and fellow teaching and the service to the community are outstanding. The opportunity to lead such an outstanding division was appealing, and I have no doubt it will achieve national excellence in multiple areas over the next few years.”
Kalra will use his clinical operations, leadership and education experience to support the UofL cardiology faculty and staff as well as grow and lead the cardiovascular medicine service line across the UofL Health System.
“With Dr. Kalra at the helm of the UofL cardiology team, I am confident that we will deliver on building upon our successful history of cardiovascular care and scale new heights of innovative and accessible care for our patients,” said Kristine Krueger, professor and interim chair of the UofL Department of Medicine. “He is an experienced physician with a demonstrated history of building successful programs in academic cardiology, skilled in patient-care delivery, change leadership and lean management processes. His arrival at UofL will catalyze our progress forward in transitioning cardiology to meet our future needs.”
Jason Smith, chief medical officer of UofL Health, said Kalra will infuse new energy and talent into the cardiology units and related disciplines at UofL health.
“He is uniquely well suited to lead UofL cardiology academic group during this unprecedented time,” Smith said. “His clinical and leadership experience will be invaluable in optimizing interdisciplinary care along the continuum, as consumers and clinicians navigate new paradigms in health care stemming from the recent COVID-19 pandemic and new models of cardiovascular care delivery. The new chief will shape the growth of cardiovascular services and, in collaboration with community cardiology leaders, will be intimately involved in developing and executing a strategic plan for integrated cardiovascular care across the UofL Health system.”
Kalra is a graduate of All India Institute of Medical Sciences where he completed his MD with honors. He then completed his residency in internal medicine in the MERIT pathway at Baylor College of Medicine in Houston. He stayed on for his fellowship in cardiology at Baylor, graduating with advanced training in cardiac imaging (echocardiography and nuclear cardiology). Prior to his arrival UofL and term at Rush, Kalra served at Baylor College of Medicine and Lahey Clinic. He is board-certified in cardiology, cardiovascular CT and MRI, echocardiography, nuclear cardiology and lipidology.
UofL School of Medicine residency program fuels physician supply for smaller communities, while offering career options to new doctors
Glasgow Family Medicine Residency program 2021 graduates, left to right, Dillon Pender, Lauren Hansen, Laura Inabnitt and Emily Marsh.
While Elizabethtown, Kentucky, native Dillon Pender was a medical student at the University of Louisville, he realized that life and medical practice in an urban setting were not a good fit for him.
So, he chose a family medicine residency program that was close to his hometown and offered the environment of a community-based hospital.
“The Glasgow Family Medicine Residency is the best of both worlds,” Pender said. “As part of UofL, it offers the privileges and resources of a major institution, and as a community hospital, it provides the autonomy you can only have outside a large health care system.”
And now that Pender has completed his residency, he plans to stay in Glasgow, serving as a hospitalist at T. J. Samson Community Hospital and caring for the community’s population. That is a win both for the community of Glasgow and the Commonwealth of Kentucky.
A shortage of physicians has threatened the health of residents in rural communities in Kentucky for more than three decades. Approximately 40% of Kentuckians live in rural areas, yet only 17% of primary care physicians practice there, and Kentucky ranks 43rd nationally in its supply of primary care physicians relative to its population.
Primary care physicians – those in family medicine, internal medicine, pediatrics or other general health disciplines – ensure access to cost-effective management of illness and disability. Since more than half of physicians practice within 100 miles of where they do their residency training, it is important for physicians to train in the smaller communities where they are needed.
The UofL School of Medicine leads two family medicine residency programs in smaller communities in the state so that small and rural communities in Kentucky and beyond have access to primary care physicians.
The Glasgow Family Medicine Residency Program trains resident physicians in the south-central Kentucky community of approximately 14,000, preparing them to practice in a similar small or rural community. Glasgow’s T.J. Samson Community Hospital is the primary clinical training site for the residency program and was named one of the Top 100 Rural & Community Hospitals for 2021 by the Chartis Center for Rural Health.
R. Brent Wright, associate dean for rural health innovation at UofL, was director of the Glasgow Family Medicine Residency Program from 2002 to 2013.
“In terms of a residency program, if you have a community that embraces graduate medical education, like Glasgow has done, they are taking a long-term approach for serving their stakeholders, ” Wright said. “They are making a commitment to those they treat for decades to come. They know that by training physicians in a close-knit and caring community, they will most likely stay within that community, close by or in a similar setting.”
The program’s 24-year track record bears out its mission. Approximately 70% of the more than 80 physicians who have completed training in the program still practice within a 90-minute drive of Glasgow, including Wright, Pender, a 2021 graduate, and Kara Gilkey, who now leads the hospital’s emergency department.
Building on the success of the Glasgow program, Wright assisted with the creation of the University of Louisville Owensboro Family Medicine Residency Program, launched in 2020. As the academic sponsor for the program, UofL provides not only experience, but residency director Jon Sivoravong and other faculty. The three-year program currently has 13 residents and is approved for up to 18, graduating an average of six family medicine physicians per year.
UofL medical students also can become familiar with rural medicine during their medical school years. Through the School of Medicine’s Trover Rural Track, UofL medical students can complete their final two years of medical school in Madisonville, a community of about 20,000 in southwestern Kentucky. Currently, 51% of Trover students who have completed their training initially chose a rural practice, and 48% of students from rural Kentucky are now in a rural Kentucky practice.
“To get physicians to practice in a small town, you have to admit students who are from a small town and train them in a small town,” said William Crump, associate dean of Trover Campus for the UofL School of Medicine.
Crump and his colleagues at UofL and Baptist Health Madisonville also prepare students from rural Kentucky communities for careers in health care through the High School Rural Scholars and College Rural Scholars programs. Of the 290 students who have participated in High School Rural Scholars, 75% have completed some type of health career training program. Of 97 students who have completed the College Rural Scholars program, 50 are either enrolled or have graduated from medical school.
For Pender, living and practicing in Glasgow is the right choice. He said many physicians who practice in urban areas are missing out on great opportunities in smaller communities, citing less traffic, a lower cost of living and friendlier people, as well as a wider scope of practice for primary care physicians since access to sub-specialty care is not as readily available.
“For most of the physicians in an urban environment, the countryside is not on their radar. They think there is nothing here,” Pender said. “But there is a lot of opportunity here and you can make a good life.”
 Facebook
Facebook Twitter
Twitter Linkedin
Linkedin