David A. Scott, PhD
 Clinical Educator
Clinical Educator
Department of Oral Immunology and Infectious Diseases
Phone: 502-852-8905
Email: david.scott@louisville.edu
Research Interests:
Tobacco, marijuana, inflammation and periodontal diseases
Periodontitis is a common inflammatory disease defined by the irreversible destruction of the supporting tissues of the teeth. Tobacco and cannabis smoking are critical risk factors for this and other chronic bacterial-induced inflammatory diseases. The mechanisms by which smoking contributes to increased susceptibility to periodontitis, and to systemic inflammatory diseases with common etiology, need to be clarified. Thus, novel therapeutic strategies can be identified. We are particularly interested in (a) how oral bacteria, primarily Porphyromonas gingivalis, survive in a tobacco-rich environments; (b) how tobacco-induced genotypic and phenotypic alterations to oral bacterial pathogens change how such microbes are recognized by the immune system; and (c) how tobacco- and marijuana-derived molecules erroneously activate endogenous anti-inflammatory pathways, such as nicotinic cholinergic signaling, and thus suppresses the ability of the immune system to fight off periodontal pathogens.
Current Funding
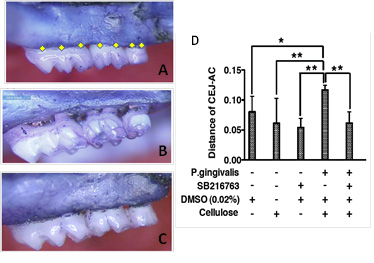
- P. gingivalis genes essential for tobacco smoke survival, R01DE026963 (P.I.)- SGK1 and the control of periodontal inflammation, R01DE026727 (Co-I):
Recent publications
Gao S, Liu Y, Duan X, Liu K, Mohammed M, Gu Z, Ren J, Yakoumatos L, Yuan X, Lu L, Liang S, Li J, Scott DA*, Lamont RJ, Zhou F, Wang H. Porphyromonas gingivalis infection exacerbates oesophageal cancer and promotes resistance to neo-adjuvant chemotherapy. British Journal of Cancer 2021. doi.org/10.1038/s41416-021-01419-5.
- Potempa J, Madej M, Scott DA*. The RagA and RagB proteins of Porphyromonas gingivalis. Molecular Oral Microbiology 2021. doi: 10.1111/omi.12345. https://onlinelibrary.wiley.com/doi/10.1111/omi.12345
Miller DP, Scott DA*. Inherently and conditionally essential proteolytic genes of Porphyromonas gingivalis. Trends in Microbiology 2021;29:54-64. doi: 10.1016/j.tim.2020.09.002. https://pubmed.ncbi.nlm.nih.gov/33071035/
- Zeller I, Malivichko M, Hurst H, Renaud DE, Scott DA*. Cigarette smoke suppresses fatty acid production by Porphyromonas gingivalis. Journal of Periodontology, 2019;https://doi.org/10.1111/jre.12660.
- Buduneli N, Scott DA*. Tobacco-induced suppression of the vascular response to dental plaque. Molecular Oral Microbiology, 2018;33:271-282.
- Hutcherson JA, Gogeneni H, Yoder-Himes D, Hendrikson E, Hackett M, Whiteley M, Lamont RJ, Scott DA*.Comparison of inherently essential genes of Porphyromonas gingivalis identified in two transposon sequencing libraries. Molecular Oral Microbiology2016;31:354-364.
- Nowicki EM, Singleton JA,Renaud DE, Colleti B, Lamont RJ, Shroff R, Ellington AD, Scott DA*, Whiteley M. Community and metatranscriptome changes accompanying the onset of gingivitis. mBio 2018;9(2).
- Roux D, Weatherholt M, Clark B, Gadjeva M, Renaud DE, Scott DA*, Skurnik D, Pier G, Lory S, Gerard C, Yoder-Himes D. A putative lateral flagella of the cystic fibrosis pathogen Burkholderia dolosa regulates swimming motility and host cytokine production. PLOS One. 2018; 13:e0189810.
- American Dental Association. Cannabis: Oral health effects. 2018; www.ada.org/en/member-center/oral-health-topics/cannabis.
- Miller DM, Hutcherson JA, Wang Y, Potempa JS, Yoder-Himes DR, Scott DA*, Whitely M, Lamont RJ. Genes contributing to Porphyromonas gingivalis fitness in abscess and epithelial cell colonization environments. Frontiers in Cellular and Infection Microbiology 2017;7:378.
- Roux D, Weatherholt M, Gadjeva M, Renaud DE, Scott DA*, Skurnik D, Priebe GP, Gerard C, Yoder-Himes D. Immune recognition of the epidemic cystic fibrosis pathogen Burkholderia dolosa. Infection and Immunity 2017:85: e00765-16.
- Simsek N, Zeller I, Renaud DE, Buduneli N, Severcan F, Scott DA*. Differentiation of chronic and aggressive forms of periodontitis by Fourier-transform infrared spectroscopy. Journal of Dental Research 2016;95:1472-1478.
- Goulas T, Ferrer I, Hutcherson JA, Potempa B, Potempa J, Scott DA*, Gomis-Ruth FX. Structure of RagB, a major immunodominant outer-membrane surface receptor antigen of Porphyromonas gingivalis. Molecular Oral Microbiology 2016:31;472-485.
- Gao S, Li S, Ma Z, Liang S, Shan T, Zhang M, Zhu X, Zhang P, Liu G, Zhou F, Yuan X, Jia R, Tai E, Potempa J, Scott DA*, Lamont RJ, Wang H, Feng X. Negative correlation between Porphyromonas gingivalis and clinicopathological characteristics and survival in patients with esophageal squamous cell carcinoma. Infectious Agents and Cancer 2016;11:3.
- Yin H, Zhou H, Kang Y, Zhang X, Duan X, Liang S, Scott DA*, Lamont RJ, Shang J, Wang H. Syk negatively regulates TLR4-mediated IFNb and IL-10 production and promotes inflammatory responses in dendritic cells. BBA General Subjects 2016;1860:588-598.
- Gu Z, Lamont GJ, Lamont RJ, Uriarte S, Wang H, Scott DA*. Resolvin D1, resolvin D2 and maresin 1 activate the GSK3b anti-inflammatory axis in TLR4-engaged human monocytes. Innate Immunity 2016;22:186-195.
- Wang H, Graves II M, Zhou H, Gu Z, Lamont RJ, Scott DA*. 2-Amino-4-(3,4-(methylenedioxy)benzylamino)-6-(3-methoxyphenyl)pyrimidine is an anti-inflammatory TLR-2, -4 and -5 response mediator in human monocytes. Inflammation Research2016;65:61-69
MAJOR COLLABORATORS
Drs. Richard Lamont, Jan Potempa and Huizhi Wang (Oral Immunology and Infectious Diseases, UofL).
Dr. Debbie Yoder-Himes (Biology, UofL)
Dr. Nurcan Buduneli (Periodontics, Ege University, Turkey).
Dr. Jackie Singleton (Dental Hygiene, UofL)
Graduate students
Graduate students who wish to pursue a M.Sc. in Oral Biology or Ph.D. (Microbiology & Immunology; Pharmacology & Toxicology; or Interdisciplinary Studies) are periodically accepted. Interested individuals should email me directly.
Clinical graduate students already at University of Louisville who wish to consider undertaking the research component of their program in my laboratory should email or call into the lab (School of Dentistry, Room 260) in person.