Research Laboratories
Neural Plasticity
Our primary research aim is to understand neural mechanisms responsible for human locomotion and the level of plasticity after neurologic injury. The primary focus is to study the plasticity of the human lumbosacral spinal cord in individuals with spinal cord injury during locomotor training. We step individuals on a treadmill with body weight support and manual assistance to maintain the normal kinematics and kinetics of walking. Locomotor training is based on providing appropriate sensory information specific to locomotion to the neuronal circuits in the spinal cord.
Neurosignalling
The research is concentrated on identification of molecules controlling neuronal/oligodendrocyte survival and growth. Of particular interest are: Area 1- Defining the role of the nucleolus in neuronal health and disease, and, Area 2- Identifying signaling pathways that control neuronal/oligodendroglial cell survival and growth.

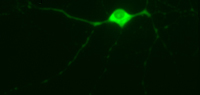
Neural Physiology & Plasticity
We investigate the cellular and molecular mechanisms regulating anatomical and electrophysiological plasticity of neurons, focusing on the peripheral nervous system and spinal cord. We are particularly interested in the interaction between, and co-regulation of, the anatomical and electrophysiological properties of neurons. We study these principles in the context of spinal cord injury and the spinal pain system (particularly in the context of damage to peripheral tissue which is a common and chronic issue for the SCI population and is an etiological factor in the development of chronic pain).
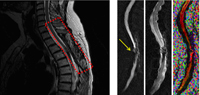
Neurosurgical Outcomes and Translational Research (NOTR) Laboratory
Research in the NOTR laboratory evaluates neurosurgical outcomes and performs population-based studies using large administrative databases. Databases include VA NSQIP and PTF databases, Marketscan, Medicare, nationwide inpatient sample (NIS), state inpatient databases and cancer registries.

Advanced Optical Imaging
The Advanced Optical Imaging laboratory uses advanced optical imaging techniques (e.g., two-photon spectral microscopy) to investigate intrinsic and extrinsic mechanisms of white matter degeneration in living tissue following trauma to the nervous system. A major thrust in the laboratory is to understand the role of microglia, the immunocompetent cells of the CNS, and blood-derived immune cells (neutrophils and monocytes) in central myelinated fiber degeneration following spinal cord injury (SCI).
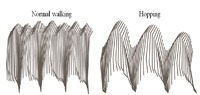
Neural Plasticity, Repair and Functional Recovery
My research focuses on understanding the response of the spinal cord to injury and identifying approaches to enhance repair, plasticity and motor recovery. At the basic science level, we have placed significant effort on the study of the chondroitin sulfate proteoglycan family and an enzyme, chondroitinase abc, which alters their growth inhibitory nature. In addition to cellular and molecular assessments to understand changes in protein expression, spinal circuitry and long tracks, we evaluate functional changes using several approaches including 3D kinematic assessment of locomotion. At the clinical research level, our major focus is on enhancing motor recovery using activity-based interventions.
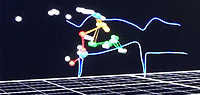
Locomotor Systems and Rehabilitation
The research in my laboratory is focused on the neurons and pathways in the spinal cord that are responsible for locomotion, and on applying what we learn about locomotor systems to spinal cord injury and repair. One of our primary investigations is focused on the long propriospinal neurons and pathways in the spinal cord that link the lumbar and cervical enlargements. A second major project in my laboratory is aimed at gaining a better understanding of activity-based rehabilitation, one of the primary rehabilitation strategies used clinically, that usually takes the form of body-weight supported treadmill training.
