Female Pelvic Medicine & Reconstructive Surgery
UofL FPMRS Surgery Youtube Channel: University of Louisville Urogynecology - YouTube
UofL Urogynecology Instagram: @louisvilleurogyn
Overview
The University of Louisville Female Pelvic Medicine and Reconstructive Surgery Fellowship is an accredited three-year program that provides comprehensive training to diagnose and treat conditions of pelvic organ prolapse, urinary and fecal incontinence, voiding and defecatory dysfunctions. Surgical education includes vaginal, open, laparoscopic, robotic techniques, and training on the DaVinci Robotic Surgical System.
 Unique opportunities include a laparoscopic dry lab and a fresh tissue human cadaver lab with full laparoscopic set-up. Specialty specific and departmental didactics are attended weekly. Fellows serve as mentors to students, residents and peers during outpatient clinics and surgical procedures.
Unique opportunities include a laparoscopic dry lab and a fresh tissue human cadaver lab with full laparoscopic set-up. Specialty specific and departmental didactics are attended weekly. Fellows serve as mentors to students, residents and peers during outpatient clinics and surgical procedures.
Twelve months of the fellowship are dedicated solely to research where basic science and clinical research are conducted in coordination with faculty mentors. Fellows are educated regarding grant writing, database creation and analysis, scientific writing, and presentation. All fellows complete a thirteen-week course in research and statistics provided by the Department of Bioinformatics & Biostatistics during the end of their first year.
One to two professional conferences are attended annually with submission and presentation of original research. Prior to graduation, fellows are expected to publish at least three peer-reviewed articles, complete a thesis project, present at at least one national meeting and sit for the subspecialty ABOG exam.
PROGRAM AIMS
- Maintain faculty that hone knowledge and skills, are active in research, provide quality mentorship based on current evidence-based practices and model professional behavior.
- Develop competent clinicians with the knowledge, clinical and surgical skills necessary to practice independently.
- Produce academicians who model professional behavior, are able to relay medical knowledge to future learners and serve as mentors during office based clinical practice and surgical procedures.
- Maintain a culture of inquiry, research, and scholarly activity that prepares fellows to independently design, implement, and analyze research for presentation and publication in peer-reviewed journals.
SUPPORTING FACULTY
Department of OB/GYN & Women’s Health
Division of Minimally Invasive Gynecologic Surgery
Resad Pasic, MD, Fellowship Director
Department of Urology
Murali Ankem, MD, Chair
Department of Surgery
Division of Colon and Rectal Surgery
Jeffrey R. Jorden, MD
Russell Farmer, MD
Sandy Kavalukas, MD
School of Public Health and Information Sciences
Department of Bioinformatics and Biostatistics
Jeremy Gaskins, PhD
Department of Medicine
Division of Gastroenterology, Hepatology and Nutrition
Thomas Abell, MD, Chair, Gastroenterology
Private Practice Physician
Urogynecology Specialists
Susan Tate, MD
Specialty: OB/GYN, FPMRS Board Certified
Baptist Health
Nechol Allen, MD
Specialty: Colon and Rectal Surgery
Nurse Practitioners
UofL Department of OB/GYN & Women’s Health, FPMRS Division
Alyce Goodman Abraham, APRN, WHN
Claire Hagan, APRN
Carrie Thonen, APRN
Dr. Lenger discusses female pelvic health on Kentucky Health
https://ket.org/program/kentucky-health/pelvic-prolapse/
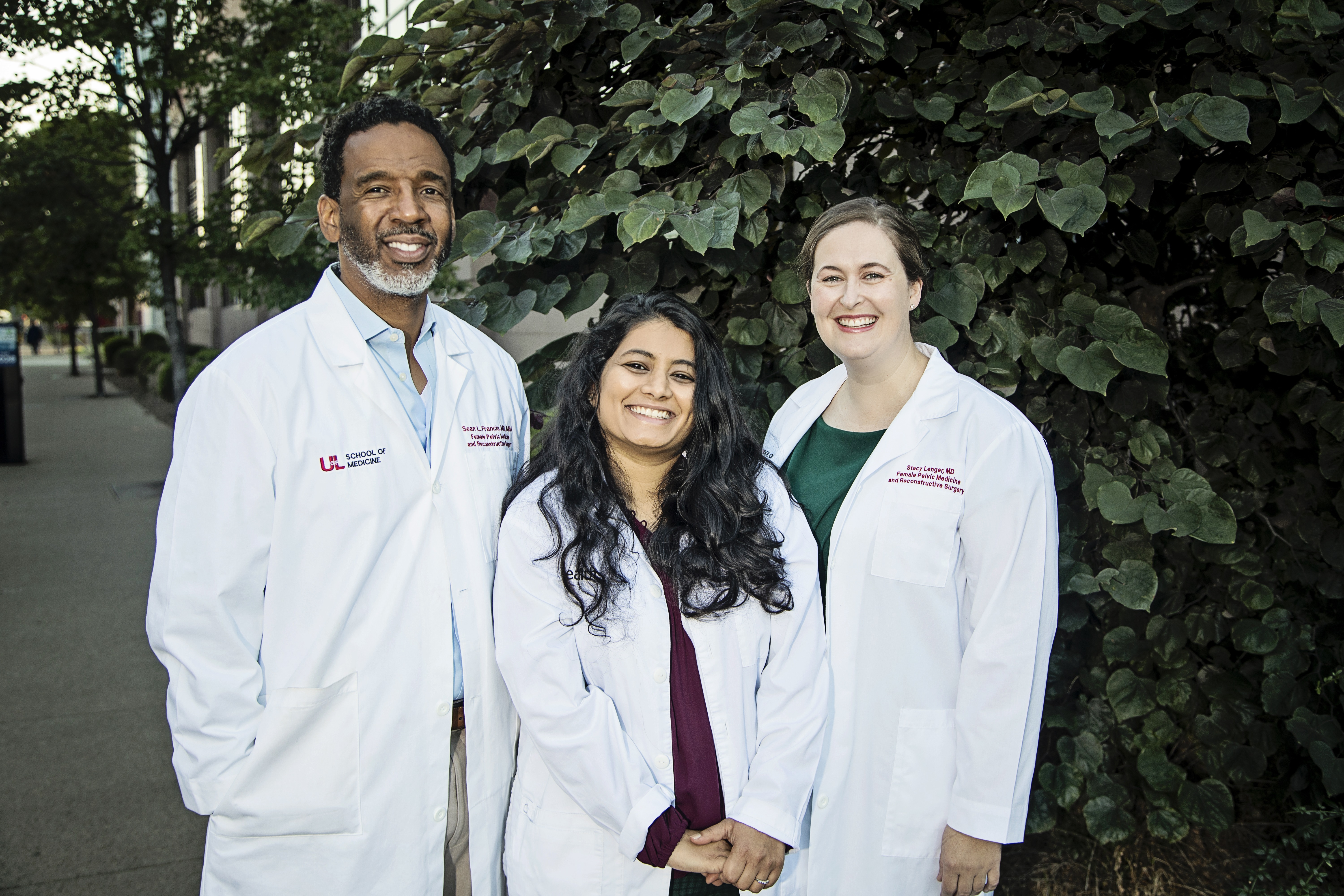
FPMRS Faculty SGS Awards 2023
Stacy M. Lenger, MD
AJOG Impact Award: D-mannose vs other agents for recurrent urinary tract infection prevention in adult women: A systematic review and meta-analysis

Ankita Gupta, MD, MPH
Rising Star Award

CURRICULUM
PGY5
The focus of the first year of fellowship training is to develop a comprehensive knowledge base in the subspecialty. Fellows work under direct supervision of faculty attendings in the office setting in completing history and physical examinations with attention to pelvic floor defects, urinary and fecal incontinence, and other benign gynecologic pathology. The fellow is introduced to the care of aging women with cognitive decline.
The fellow also works closely with faculty attendings in the operating room and inpatient units providing pre- and post-operative surgical care. Under direct supervision, the fellow conducts pre-operative evaluations, participates in surgery and rounds on post-operative patients on the service. The goal is for the fellow to develop good surgical technique in the operating room such as the
The fellow develops appropriate professional attitudes and behaviors and provides teaching in both informal and group discussions with third- and fourth-year medical students and second-year residents, as well as other trainees rotating on the service. An understanding is developed with respect to partnering with health care managers and other health care providers to assess, coordinate, and improve health care. Specifically, fellows function as a role model for colleagues and medical students on service.
Finally, the fellow demonstrates the use of current written or electronic information as an adjunct to the care of patients.
Research time is devoted to developing a research proposal and timeline and to obtain IRB approval.
PGY6
With increasing proficiency, the second-year fellow effectively manages more complex cases of prolapse and incontinence, coordinates patient care, and continues to develop the necessary skills to function as an effective subspecialist. Skills include appropriate utilization of personnel and resources, which includes the understanding of personal limitations.
The fellow gains knowledge in the initial evaluation of patients presenting with fecal incontinence and various forms of colon and rectal problems. S/he participates in pre-operative evaluations, completion of history and physical examinations with attention to rectovaginal fistulas, hemorrhoids, bowel anastomosis, rectal prolapse and other pathology related to the colon and rectum.
Under direct supervision, the fellow participates in surgery and rounds on post-operative patients on the service. The PGY-6 fellow becomes more proficient with technical skills acquired during the previous year of training and expands clinical experience in pre- and post-operative care of patients with pelvic organ prolapse.
The PGY-6 fellow’s ability to serve as a source of medical knowledge and to perform as a teacher increases as the fellow trains residents and medical students on the service.
The fellow strives to make independent decisions while under supervision earning the trust of colleagues. Workload is greater than during the previous year of fellowship, with increasing responsibility, so the development of good time management, communication, and professional skills is essential.
Time is devoted to the initiation of research projects outlined and approved during the first year of fellowship with completion and publication during the final year of fellowship.
PGY7
All training in the previous two years culminates in the final year of responsibility and competence, thus the goal for completion is to demonstrate the knowledge and skills necessary to practice independently upon completion of the program. The PGY-7 fellow is primarily responsible for diagnosis and development of a care plan for each patient; s/he manages the treatment and performs as primary surgeon with faculty attendings in the assistant’s role in all FPMRS surgeries for pelvic floor defects, urinary and fecal incontinence, and other benign gynecologic pathology.
Fellows perform non-surgical techniques to treat different anomalies, perform surgical techniques (including Vecchieti procedure) to treat urogenital anomalies and know appropriate timing and indications for gonadectomy. The fellow also becomes proficient on neuro-urology and neuromodulation and develops competency in advanced laparoscopy and robotic surgical technique.
The fellow demonstrates a level of competence in cadaveric dissection and subspecialty whereas s/he can now teach independently. The PGY-7 functions at the level of an attending in Female Pelvic Medicine and Reconstructive Surgery.
The PGY-7 demonstrates competence in research with presentation and acceptance of thesis and submission of research manuscript for publication in the peer-reviewed literature. On site, the research is presented at the departmental annual Research Day.
Research
Fellows will participate in scholarly activities based on their areas of interest both within the institution and at the national level. Fellows will spend a total of 12 months of protected time for research during fellowship.

The PGY 5 fellow will participate in and successfully complete the 12-week OB/GYN Fellowship Research and Statistics Course conducted by Jeremy Gaskins, PhD, Biostatistician. Fellow will participate in grant writing as appropriate under the guidance of the research mentor. Fellows are encouraged to publish at least three times in peer reviewed journals and present their work at scientific meetings. All fellows attend the annual American Urogynecologic Society scientific meeting as well as other scientific meetings throughout the year that they have works accepted to present.
In addition to clinical education, the goal of the fellowship program is to advance fellows’ skills as physician-scientists. While the ability to create new knowledge within medicine is not exclusive to fellowship-educated physicians, the fellowship experience expands a physician’s abilities to pursue hypothesis-driven scientific inquiry that results in contributions to medical literature and patient care. Beyond the clinical subspecialty expertise achieved, fellows develop mentored relationships built on an infrastructure that promotes collaborative research.
Fellows will participate in scholarly activities based on their areas of interest both within the institution and at the national level. Fellows will spend a total of 12 months of protected time for research during fellowship.
During the fellow’s research block month, no more than four hours of a fellow’s time each week (averaged over a four-week period) will be devoted to non-research activities. During research blocks, the fellow’s mentor(s) will be available to answer research questions and to aid in the development and execution of the research project.
Fellows are expected to be prepared to present and discuss their progress regarding research during the monthly FPMRS Research Meetings.
Research Day is held each spring, the first Friday in June and attendance is required. The third-year fellows for present their thesis projects. The third-year fellow gives an oral presentation with a PowerPoint document. A visiting lecturer presides over the day. This exercise gives fellows an opportunity to develop their research and presentation skills and demonstrate their expertise to community physicians.
Didactics
The fellowship is the cornerstone of the Female Pelvic Medicine and Reconstructive Surgery division, which is committed to a strong teaching curriculum for members of the department and school of medicine, including faculty, residents, and medical students.
As part of our educational mission, the division conducts:
- weekly didactic course based on objectives outlined in the Guide to Learning in Female Pelvic Medicine and Reconstructive Surgery, American Board of Obstetrics and Gynecology (ABOG)
- weekly pre- and post-operative conferences
- monthly subspecialty journal club
- quarterly colorectal conference
- quarterly FPMRS M&M conferences
- AUGS Fellow Webinars
At the weekly seminar/didactic courses, fellows present assigned textbook chapters and preselected articles under the direction of a faculty mentor.
Fellows attend the department’s weekly Grand Rounds presentations, pertinent weekly Continuous Quality Improvement, preoperative gynecology conferences, morbidity and mortality conference, and Journal Club, all held within protected educational time.
Fellows present a Grand Rounds topic each academic year and conduct resident didactics during each year of training.
Requirements for Graduation
To graduate from the Female Pelvic Medicine Fellowship Program at the University of Louisville, fellows are expected to meet the following milestones:
- Completion of curriculum requirements, goals and objectives outlined.
- Attendance and participation in monthly FPMRS Research Meetings.
- Publication of three articles in peer-reviewed publications.
- Presentation at least once at a regional, national, or international meeting or conference.
- Completion of thesis that meets guidelines outlined by ABOG.
- Presentation of Research Thesis during PGY 7 Year at Research Day in June.
- Submission of thesis Research Day slide presentation and completed manuscript.
Benefits and Perks
STIPENDS AY 22-23
Stipends are determined by the Graduate Medical Education (GME) Office prior to the beginning of each academic year. Fellows will be provided a new contract each academic year. Stipends for Academic Year 2022 - 2023 are as follows:
PGY | STIPEND | |
5 |
| |
6 |
| |
7 |
|
HEALTH INSURANCE
University of Louisville benefits can be located at the following link: http://louisville.edu/hr/employment/newemployee/benefits.
MALPRACTICE INSURANCE
The department pays for fellow malpractice insurance through Kentuckiana Medical Reciprocal Risk Retention Group (KMRRRG).
DEVELOPMENT FUNDS
The following amounts will be available for expenditure between July and June each academic year:
Fellows | $2,000 annually (July 1 – June 30) PLUS:
PLUS:
|
GYM MEMBERSHIPS
Faculty/Staff Student Recreation Center Membership
Faculty, staff, and retirees of the University are eligible for memberships to the new Student Recreation Center. The cost is only $24 per month and is available in monthly increments from 1 to 12 months. Dependents of members are eligible for memberships at the same rate as the original member. For a dependent to join, the host must be a member for a period of time equal to or greater than the length of time desired for the dependent.
https://louisville.edu/studentaffairs/forms/ubm/intramurals-src-membership
HSC FITNESS CENTER
Elliptical trainers, treadmills, stationary bikes, recumbent bikes, and stair climbers comprise the complete line of cardiovascular equipment at the Health Science Center (HSC) Fitness Center. The center also features a complete line of weight stack and free weight equipment. Group fitness classes are held in the group fitness studio most days at noon and early evening. Locker Rooms with lockers and individual showers are also available. The gym is located at 416 East Chestnut Street, on the first floor of the UofL Parking Garage.GET HEALTHY NOW
Offers a wide range of wellness activities and classes: https://louisville.edu/gethealthynow/wellness-resources:
- Beginner Yoga/Chair Yoga: Pause from your busy life to recharge and revitalize at our quiet calming practice of body and breath awareness.
- Bootcamp: High intensity interval training that incorporates strength, cardio, sport movements, CrossFit, and running.
- Fit in 30!: Power up your lunchtime routine with an energizing, whole body workout, including a variety of strength and cardio moves, all in just 30 minutes! Suitable for all levels.
- Latin Dance: Laugh, dance and de-stress while learning basic Latin dances. All levels are welcome and no partner required.
- Mindful Yoga: Calm the nervous system, increase the body-mind connection, and improve breathing.
- PiYo: Combines the sculpting and core benefits of Pilates with the strength and flexibility benefits of Yoga.
- REFIT®: Moves beyond the body into a life-changing experience. Refit believes the heart is both a muscle and a soul, and the impact of this targeted approach creates a deeper sense of connection, self-worth, and lasting change.
- Tai Chi: Discover the benefits of this ancient form of martial arts, which will improve balance, agility, strength, and coordination.
- Yin/Yang Yoga: Bring an open mind and be prepared to enjoy an energizing and refreshing yoga experience – Yin yoga is slow and restorative; Yang Yoga is more powerful and challenging. Come prepared to do a mix of both!
- Zumba®: The ultimate dance-fitness party! Enjoy Latin, hip-hop, and International music and get in a great workout while you learn dynamic and effective dance moves!
CAMPUS HEALTH SERVICES
Campus Health Services for fellows are offered at no charge for immunizations and required FIT testing. Campus Health Services located in the HCOC and at Cardinal Station offers a compressive list of services designed to meet the needs of our students, residents, and fellows in training. Services are billed to the individual’s commercial insurance, workers’ compensation or covered by the GME or student fees. Generally, not out of pocket expenses.
Trainees are guaranteed a clinical site where there are no students or residents rotating in the office privacy purposes. A dedicated staff of physicians, psychiatrists, nurse practitioners, registered nurses, and certified medical assistances staff both locations.
UNIVERSITY OF LOUISVILLE EMPLOYEE ASSISTANCE PROGRAM (EAP)
An Employee Assistance Program (EAP) is available to university employees at no charge and provides confidential counseling, assessment, and referral services. The program deals with the broad range of issues such as emotional/behavioral, family and marital, alcohol and/or drug, financial, legal, and other personal problems.
How to Apply
Application Process
Applications to the University of Louisville Female Pelvic Medicine and Reconstructive Surgery Program will be accepted ONLY through the Association of American Medical College's (AAMC) Electronic Residency Application Service (ERAS). The program does not require additional documentation to complete application.

- All required clinical education for entry into ACGME accredited fellowship programs must be completed in an ACGME accredited residency program.
- For an international Medical School graduate, verification of Educational Commission for Foreign Medical Graduates (ECFMG) certification will be required.
- Our program does accept J1 Visa applicants as long as the applicant has three years remaining on their visa in order to complete the fellowship.
Important Dates
We will be interviewing virtually. Interview dates for the upcoming interview season are April 17, 2024 and May 15, 2024.
FPMRS Fellowship Application: Key Dates | |
11/15/2023 | ERAS opens for application submission. |
12/6/2023 | Programs will begin to review applications. |
1/22/2024 | Application deadline for consideration of first round of interview offers by participating urogynecology programs |
| 2/12/2024 | Programs will send out first-round interview invites by 8:00 p.m. ET |
| 2/19/2024 | Deadline for applicants accept or decline first round interview invite. |
| 4/17/2024 | University of Louisville Interview Day 1 |
| 5/15/2024 | University of Louisville Interview Day 2 |
| 5/31/2024 | Interview Season Ends |
WHY LOUISVILLE?
Click the links below for information about the city of Louisville
City of Louisville - Louisville is a progressive community of nearly 1 million people. Many residents live in areas that have the feel of a neighborhood but are conveniently located very
close by the hospitals where they work. Situated on the banks of the Ohio River, America's 17th largest city boasts a cost of living that is substantially lower than the national average, with a broad range of affordable housing options from high-rise apartments and historic Victorian homes to suburban communities and rural farms.
Louisville is best known for a variety of things including the world-famous Kentucky Derby, bourbon and its diverse dining options. In fact, there are so many great places in Louisville to grab a
meal from, Travel and Leisure magazine recently ranked the Derby City as one of the top 10 destinations in the United States for foodies! Professional opera? Check. Professional ballet?
Sure. Professional orchestra? Yep. Professional theatre? Sure. Children’s theatre? Of course. Rounding out this list is a fabulous fact for art lovers: Louisville is not only one of a handful
of cities in the country with all of the aforementioned resident performing arts groups, but also has many renowned visual arts outlets as well, including the 21c Museum Hotel and Speed Art Museum. There are wonderful theaters, music, and galleries and festivals that occur throughout the year.
Those who love playing outdoors should feel at home in Louisville, which has some of the most parkland per capita in the country. The city’s parks system comprises more than 15,000 acres, and it’s especially attractive since much of it was designed and planned by the Father of American Landscape Architecture, Frederick Law Olmsted. The system is one of only four Olmsted designed (he also designed New York’s Central Park) and includes a total of 18 parks and six parkways that he and his successor firm developed. There are many more public recreation spaces beyond these, as well, including many miles of paved trails for biking, walking and running.
Louisville was one of the first city in the South to pass a LGBTQ+ Fairness Ordinance, and Louisville Metro Government was one of the first Southern cities to extends benefits to employee's domestic partners. The University of Louisville maintains five stars in the Campus Pride Index and was the first public university in the South ranked among the “Best of the Best.” Our medical school also piloted the first medical student training for targeted LGBTQ healthcare needs, and it was the first university in the country to offer a LGBTQ+ Studies minor. Louisville offers the amenities of a city but with the welcoming atmosphere of a town.
The Health Sciences Center has their own Office of Diversity and Inclusion at the University of Louisville and welcomes and embraces our community of students, residents, fellows, faculty, and staff. By augmenting a culture and climate that demonstrates its belief that diversity and inclusion adds value to intellectual development, academic enrichment, patient care, research, and community engagement, we believe our campus will be at the forefront of opportunity and innovation. The HSC Office of Diversity and Inclusion's goal is to enhance partnership across the schools on the Health Sciences Center campus as we continue to promote an environment of inclusiveness through the understanding and celebration of the many differences in perspectives, thoughts, experiences, belief systems, and cultures of our students and employees.
Contact Information
Dana Lamon, Fellowship Coordinator
Department of Obstetrics, Gynecology & Women's Health
University of Louisville School of Medicine
550 S. Jackson Street
Louisville, KY 40202
(502) 561-7260
