Rotations
Sample Block Schedule
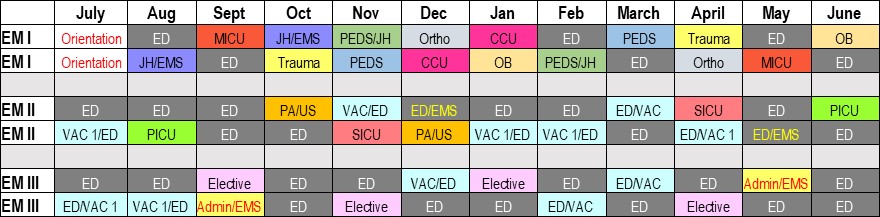
INTERN YEAR
Orientation (University Hospital) – 1 month
- All 12 interns begin their year working 10 shifts to acquaint themselves to the department and take part in orientation didactics
- ATLS, ACLS, and PALS certifications obtained this month
- A tour of community health clinics, EMS/Fire day, resident manual overview, and EMR/dictation training, and wellness activities will be arranged
- The month is full of social events to meet your colleagues, faculty, and staff!
Emergency Medicine (University Hospital) - 3 months
- See a wide range of chief complaints and acuity, present to senior residents with faculty oversight
- Assist in cardiopulmonary and trauma resuscitation available every shift
- Learn procedures such as intubation, central line placement, lumbar puncture, incision and drainage, and others
- One built-in week of vacation each month
Pediatric EM (Norton Children's Hospital) - 1 month + 1/2 month
- See a variety of pediatric patients under the supervision of Pediatric Emergency Medicine attendings and fellows
- This rotation takes place at Norton Children’s Hospital, a Level I Pediatric Trauma Center
- One-half month during a split Jewish/Peds month and one full month
- One built-in week of vacation during the full month
- Pediatrics shifts in residents 2nd and 3rd year are longitudinal to allow residents to see a variety of pediatric chief complaints
Community EM (UofL Health Jewish Hospital) - 1 month + 1/2 month
- Experience a high-volume, community Emergency Department with medically complex patients under the supervision by ABEM-certified Emergency Physicians
- This rotation takes place at UofL Health Jewish Hospital, a comprehensive cardiovascular care center and transplant center
- One-half month during a split Jewish/Peds month and one full month
- One built-in week of vacation during the full month
Cardiology Critical Care - 1 month
- An inpatient Cardiology rotation based out of the Cardiac Care Unit (CCU)
- This rotation emphasizes the management of acutely-ill cardiology patients, such as patients with acute heart failure exacerbation and myocardial ischemia
- EM residents will have a variety of work experiences as a member of the team, including on-call emergency department consult coverage, a week of night float coverage, and call every 3 to 5 days
Medical Intensive Care (University Hospital) - 1 month
- Evaluate and assist in the management of the critically-ill, including ventilator support and management, invasive hemodynamic monitoring in a tertiary care ICU
- Residents are supervised by Pulmonary/Critical Care fellows and attending staff
- Call every fourth day
Obstetrics and Gynecology - 1 month
- Clinical responsibilities caring for both postpartum and antepartum patients, labor and delivery patients, and evaluation and treatment of patients in the OB-triage area
- EM I residents will perform vaginal deliveries and get the opportunity to assist with Caesarean sections and gain experience in pelvic and transvaginal ultrasound
Orthopedic Surgery/Toxicology - 3 weeks/1 week, total of 1 month
- For 3 weeks of this rotation, EMI residents are assigned to an orthopedic team with Orthopedics faculty, a PGY-5 orthopedic resident, PGY-3 orthopedics resident, and orthopedics intern
- This clinical experience includes emergency department coverage to master fracture and dislocation reduction and splinting, as well as have opportunities to take part in orthopedic procedures such as hematoma blocks, joint loading, and others
- For 1 week of this rotation, EMI residents will rotate with our at the Kentucky Regional Poison Control Center under the direction of our toxicology faculty to experience case consults for acute ingestions.
Trauma Surgery - 1 month
- EM I residents rotate on the trauma service for one month and are integral members of one of two inpatient trauma teams.
- Learn the longitudinal care of the trauma patient alongside surgical attendings, a senior surgery chief resident, and a PGY-3 surgery wedge
- Assist in trauma resuscitations in the ED, with opportunities for procedures such as central venous access and tube thoracostomy alongside surgical experts
SECOND YEAR
Emergency Medicine (University Hospital, UofL Health Medical Center South , Norton Children’s Hospital) – 9 months
- Nine total one-month blocks of emergency medicine
- Pediatrics shifts at Norton Children’s Hospital compromises 20-25% of total shifts
- Approximately 15% of shifts are at UofL Health - Medical Center South, a freestanding emergency department that allows a unique clinical experience
- The majority of shifts are at University Hospital, where the EM II will take turns with the EM III on shifts as the resuscitation leader in “Room 9” medical and trauma resuscitations
- EM II residents will serve as clinical educators for both medical students, and later in the year, EM I residents
- Four total weeks of vacation is included within these nine months
Pediatric Intensive Care Unit (Norton Children’s Hospital) - 1 month
- One month as a member of the Pediatric Critical Care Team, taking care of the sickest pediatric medical and trauma patients alongside Pediatric Critical Care attendings and fellows
- Care for patients in Kentucky’s only stand-alone full-service pediatric hospital
Surgical Intensive Care (University Hospital) - 1 month
- Residents are assigned to one of two inpatient trauma teams, caring for patients in the Surgical ICU at University Hospital
- Responsibilities include caring for critically ill pre and post-surgical patients, including those that require ventilator support and invasive hemodynamic monitoring
- Supervision is done by surgical critical care fellows and attending staff
Pediatric Anesthesia (Norton Children's Hospital) - 1/2 month
- A 2-week rotation alongside an anesthesia team at Norton Children’s Hospital
- Teams consist of an attending anesthesiologist, resident anesthesiologists, and certified registered nurse anesthetists
- Residents will have multiple opportunities to learn the complexities of airway management in the pediatric population
- Procedures such as intubation, laryngeal mask airway, and proper bag mask ventilation will be done by rotating EMII residents
Ultrasound (University Hospital) - 1/2 month
- A self-paced rotation alongside our Ultrasound Directors Dr. Dan O’Brien and Dr. Jeffrey Baker during shifts at University Hospital’s emergency department
- Rotating EM II residents will learn and improve upon their point of care ultrasound skills, including cardiac ultrasound, abdominal ultrasound, soft tissue ultrasound and more
THIRD YEAR
Emergency Medicine (University Hospital, UofL Health Jewish Hospital, Norton Children’s Hospital) - 9 months
- Nine total one-month blocks of Emergency Medicine
- Pediatrics shifts at Norton Children’s Hospital compromises 20-25% of total shifts
- Approximately 15% of shifts are at UofL Health- Jewish Downtown, a busy community hospital responsible for the region’s transplant patients as well as a comprehensive cardiac center
- The majority of shifts are at University Hospital, where the EM III will take turns with the EM II on shifts as the resuscitation leader in “Room 9” medical and trauma resuscitations
- EM IIIs have increased responsibilities, learning to manage the department as whole while balancing supervising EM I residents and medical students
- Four weeks of vacation is included within these nine months
Administrative Emergency Medicine - 1 month
- One month of administrative departmental duties under the supervision of Dr. Adam Ross, the University of Louisville Emergency Department Director
- Explore the administrative tasks and operational leadership issues within the hospital’s ED
- The administrative resident performs quality improvement for the department alongside Dr. Ross, reviewing patient cases that were triggered for review in our EMR
- The EM III serves as clinical shift back-up coordinator for the department this month
Elective - 2 months
The EM III is allotted 8 weeks of elective experience. A wide array of opportunities are currently available, and the department staff is more than happy to work with the EM III to coordinate and plan an elective in an area of interest if there is not one currently available. Examples of past electives include:
- Clinical Forensic Medicine
- Medical Toxicology
- Metro Search and Rescue Team (MSAR)
- Underwater Search and Rescue
- Radiology
- Stroke
- Tactical Emergency Medicine Support (TEMS)
- Ultrasound
- Hyperbaric Medicine
- Advanced EKG
- Sports Medicine
 Instagram
Instagram
 Twitter
Twitter
 Blog
Blog